Ver evolución gráfica del caso
Complete mandibular prostheses in fully edentulate patients with major atrophy usually present difficulties in fit and mobility, affecting chewing, phonetics and aesthetics.
One treatment option in this type of case is an immediate overdenture: to fit implants with a small diameter and an implant-mounted restoration, improving levels of aesthetics, stability and prosthesis retention and consequently the patients' quality of life.
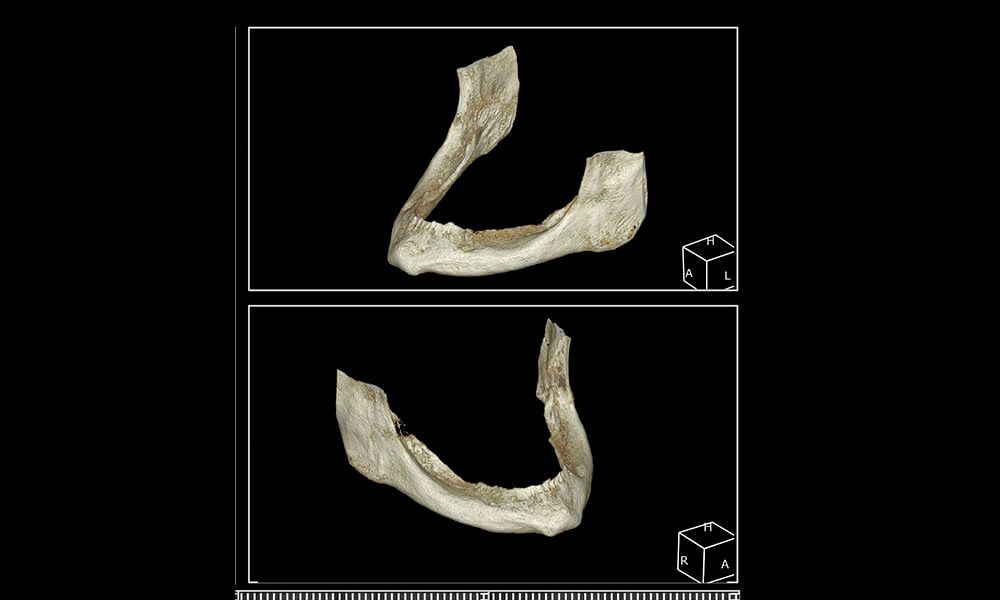
Edentulate patient aged 60 years, with no medical history of interest and all teeth removed more than 20 years ago, comes to the clinic because she cannot tolerate the mobility of her lower removable prosthesis and other clinics have told her she is not a candidate for implants due to the extreme mandibular bone reabsorption she presents.
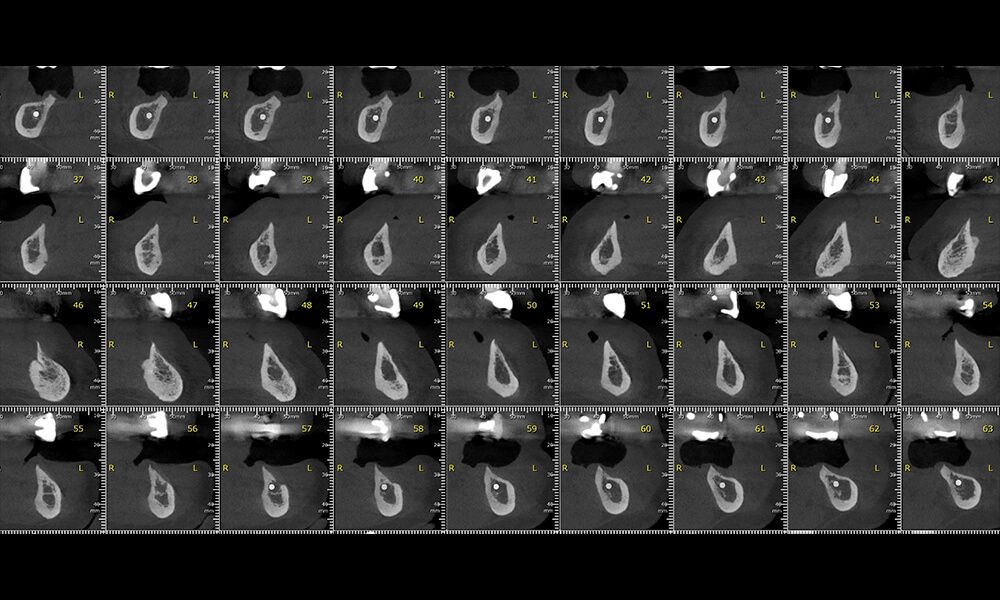
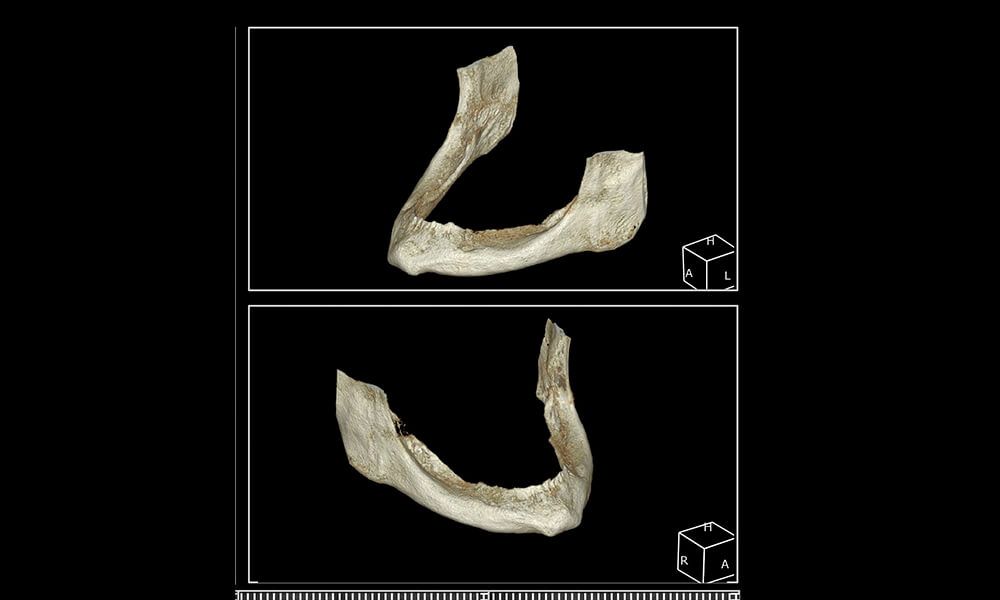
A clinical examination and CT corroborate the severe bone limitation she presents, in both height and width (images 1 and 2).
After an exhaustive clinical study, the patient ruled out the option of bone regeneration treatments to achieve the necessary bone and place conventional implants. It was then decided that the best option to solve her problem and improve her quality of life would be an immediate overdenture: to fit 4 reduced-diameter Biomimetic Pearl (Avinent) implants.
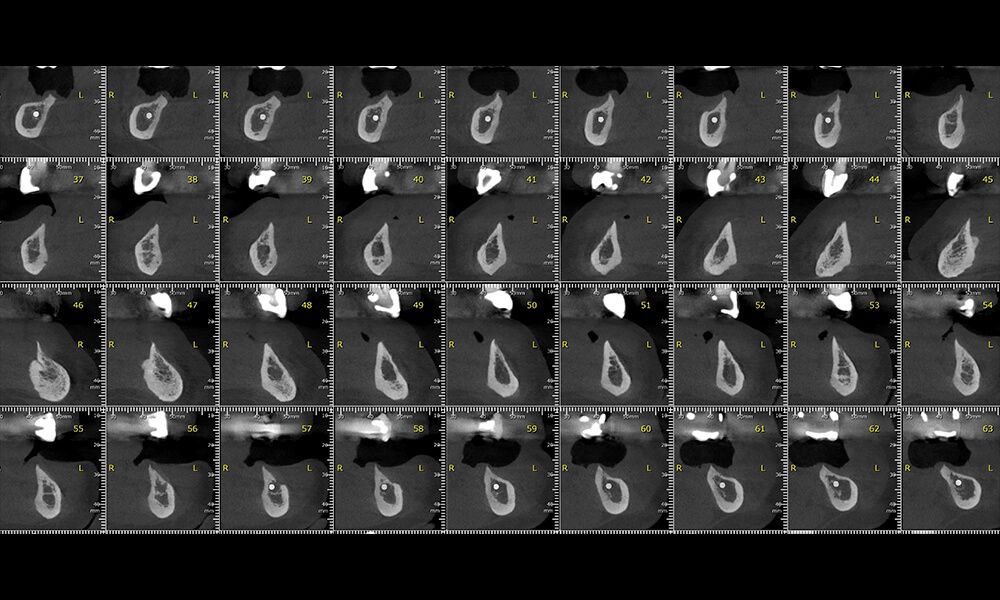

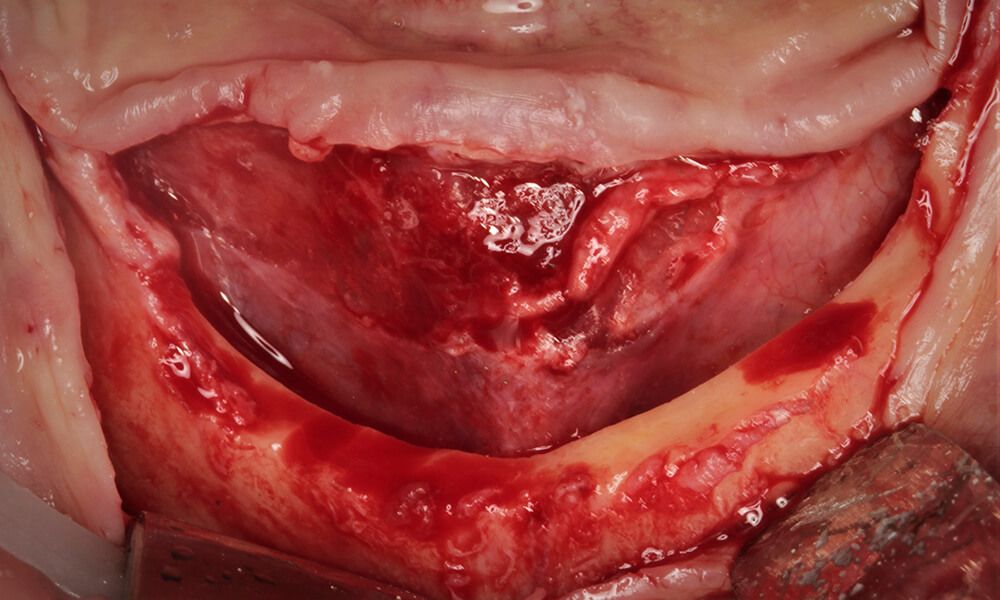
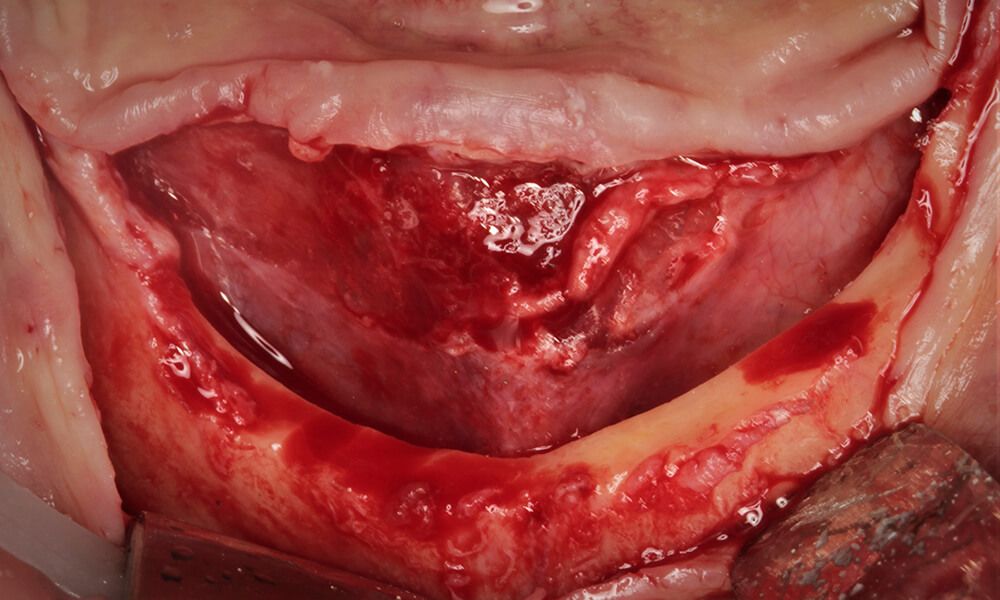
The surgery began with a longitudinal crestal incision without relief cuts, with special attention to the mental nerves that were in a crestal position due to the reabsorption and that could have been damaged. Then a full-thickness flap was detached for a better view of the anatomical aspects of the mandible. A crestal width of 1 mm was observed, which was evened until a platform of approximately 4 mm was achieved, sufficient to place the four narrow implants at the same level.
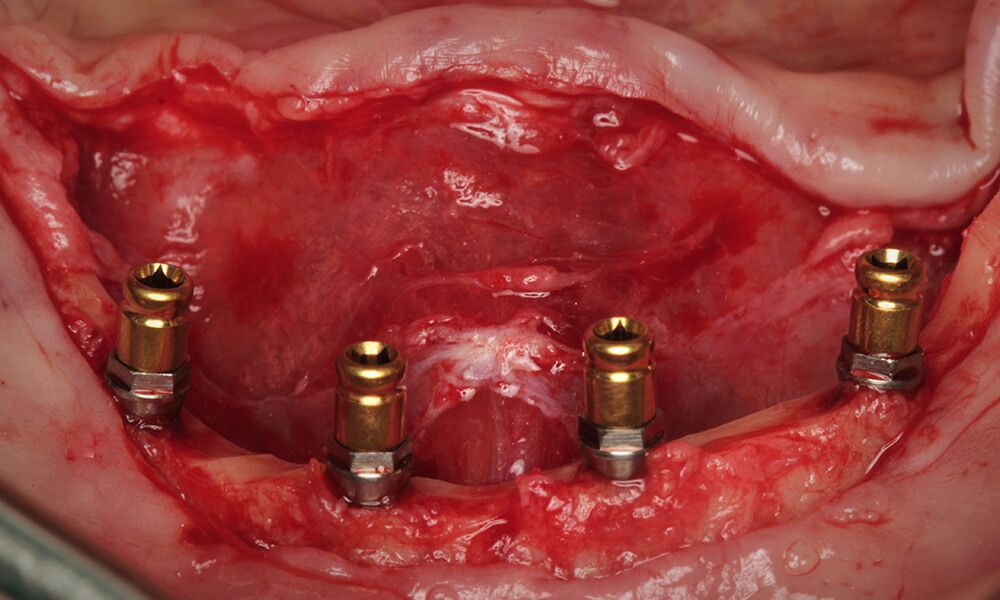
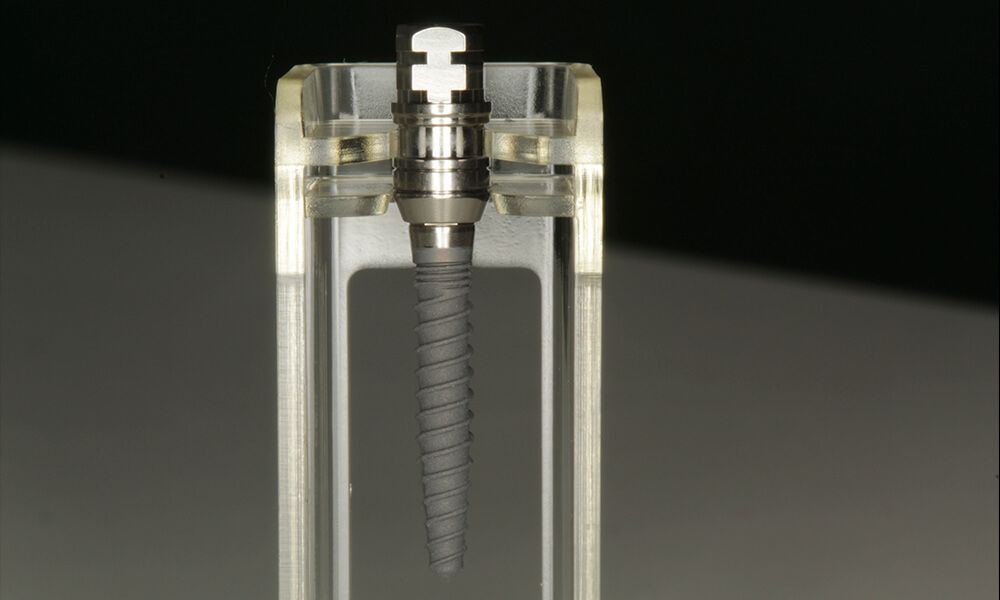
To carry out the immediate overdenture four Biomimetic Pearl implants, 2.4 mm in diameter and 11.5 mm long, were placed, seeking parallelism and bicortical anchoring with the basal area of the symphysis, achieving excellent primary stability of over 35 Ncm. They were placed so that the treated part would remain infraosseous and the polished area of the implant neck supraosseous, preventing possible subsequent bone loss.
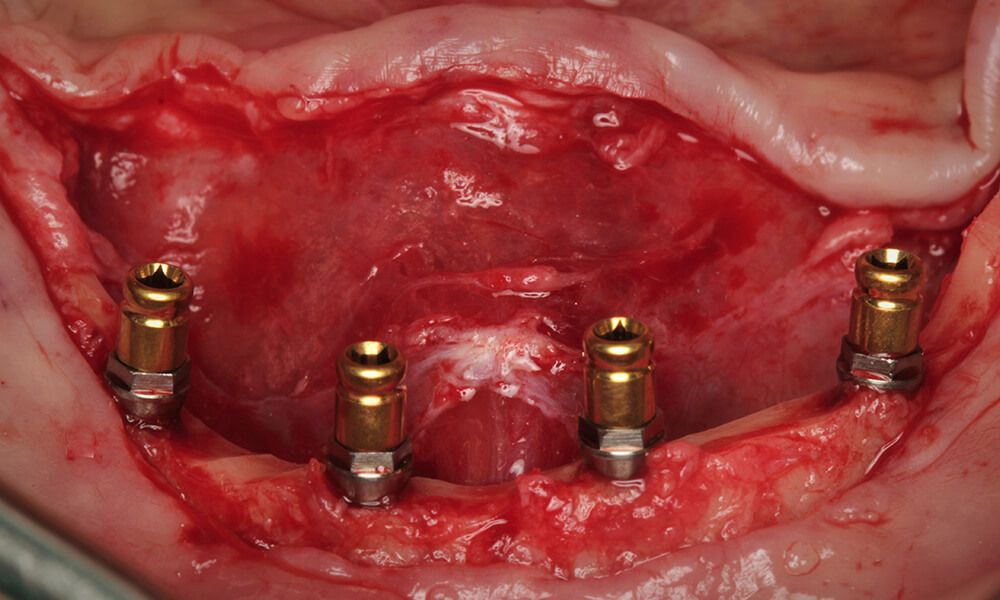
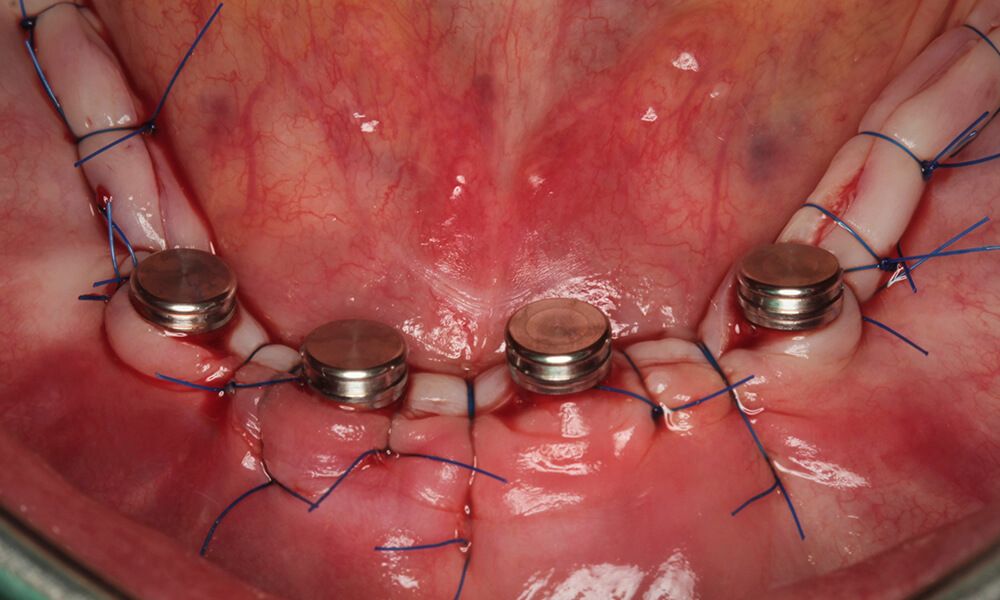
In the same surgery, a Rhein transmucosal abutment, with a height of 2.8 mm, at a torque of 25 Ncm, was screwed into each implant for overdentures. Due to the design of the Pearl mini-implant transporter, it can be used to make this process transmucosal, without disconnecting it and avoiding tissue collapse.

As we had evened the bone for implant placement, there was an excess of soft tissue that could cause problems when suturing, as a conventional suture would leave the implant abutments subgingival.
For this reason it was decided to place caps with black Teflon (extra smooth) and gain 2 mm in height and use an intraosseous suture (crossing the crest in a vestibular-lingual direction with a lance drill and passing one single stitch through the bone), to compress the soft tissue against the bone. This close contact between the periosteum and the bone enabled early healing and the preservation of what little keratinized gum was available around the cap placed on the abutments.
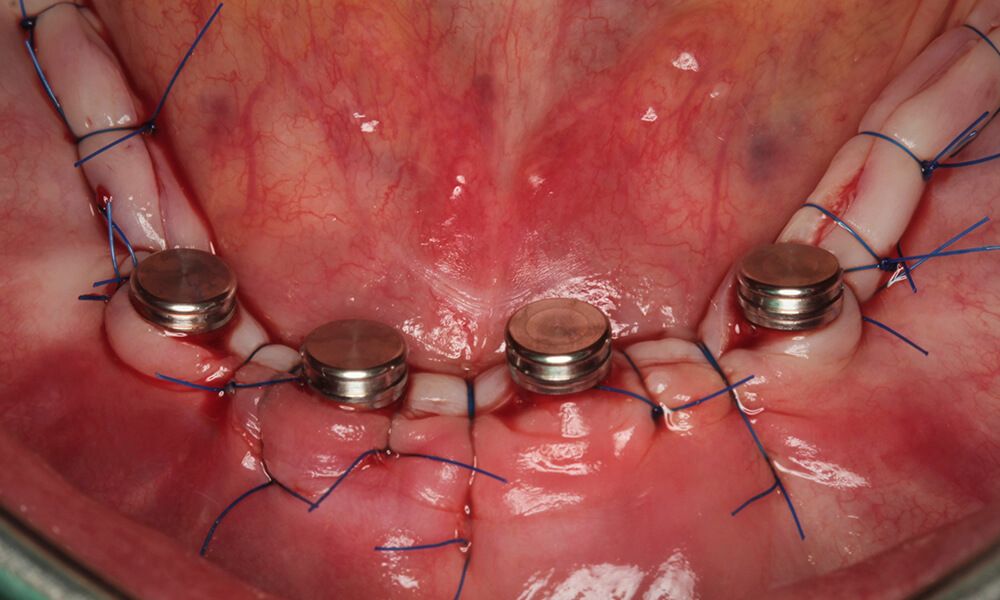
Due to the high primary stability achieved by the implants, an impression was taken immediately, taking the caps with the patient's provisional prosthesis itself. The prosthesis was left in place for 72 hours, without removing it, to stabilize the tissue.
After 2 weeks the tissues were checked and cleaned and the sutures removed.
After 3 months a definitive overdenture was made with the implants perfectly integrated.




The use of this suture technique simultaneous to fitting the abutments and caps, along with the tissue compression and immediate load, provided excellent quality soft tissues around our implants in one single surgery.

The soft tissue showed excellent affinity and behaviour, producing a gingival seal at the level of the Rhein abutment, and an absence of inflammation.


In one single surgical operation the patient's expectations were fulfilled, retaining her complete prosthesis and recovering her quality of life. This is in addition to a very good long-term prognosis due to the excellent design of the Biomimetic Pearl system, which makes quick and minimally invasive treatments possible for cases of severe mandibular atrophy, with low surgical risk and few complications compared with bone augmentation procedures.