Ver evolución gráfica del caso
Introduction
Although the number of completely edentulous patients has currently decreased, there remains a group of patients seeking treatment after losing their remaining teeth due to advanced periodontitis. In these cases, severe associated bone atrophy may complicate conventional implant treatment.
To be treated, these patients will require guided bone regeneration treatments prior to or simultaneously with implant placement to increase the alveolar ridges and improve the long-term prognosis of the treatment.
As demonstrated below, current guided bone regeneration (GBR) techniques are an excellent alternative for achieving satisfactory aesthetic results in the regeneration of peri-implant defects.
Case Presentation and Planning
A 60-year-old female patient, a former smoker with no significant medical history, visited the clinic to replace her removable partial denture with a fixed rehabilitation.
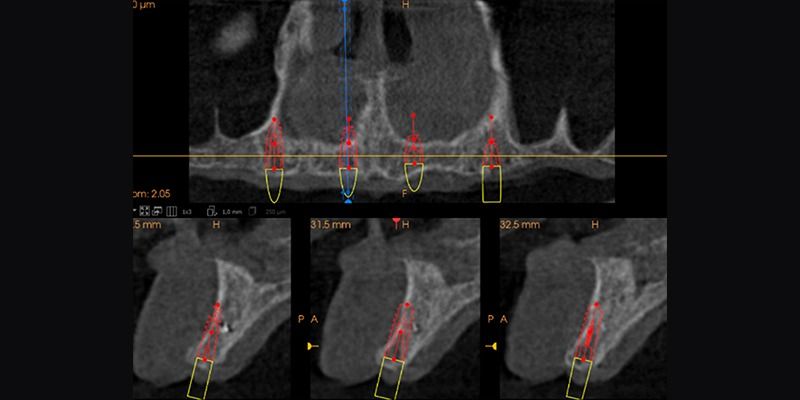
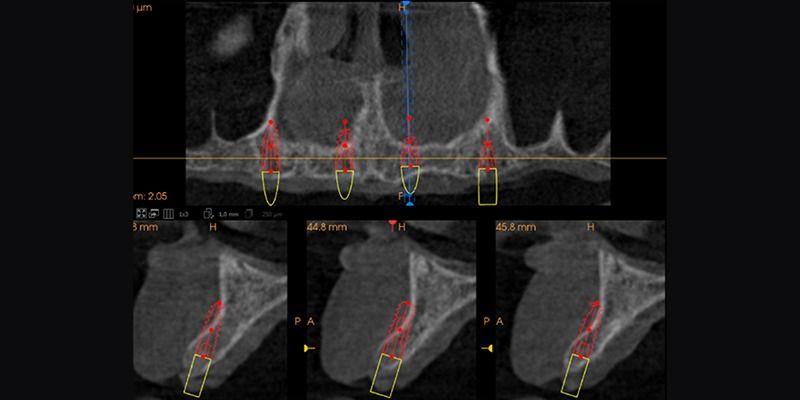
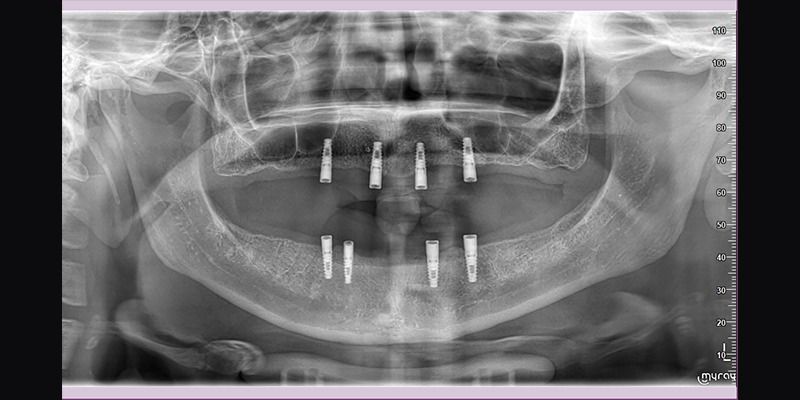
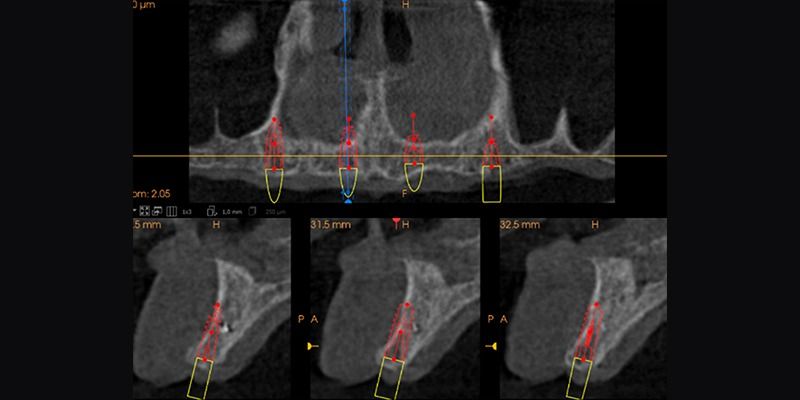
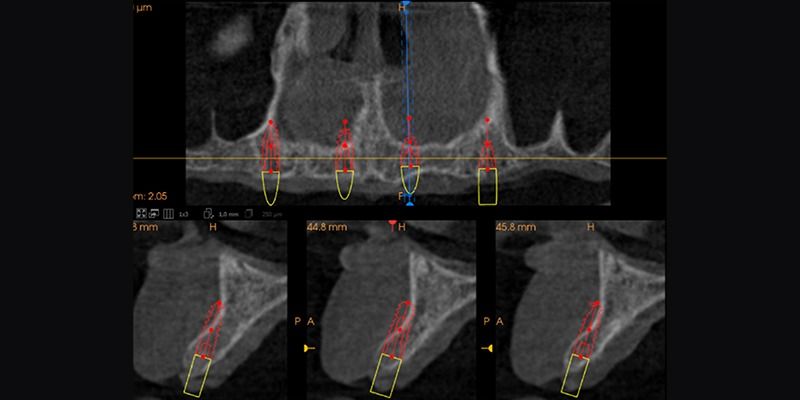
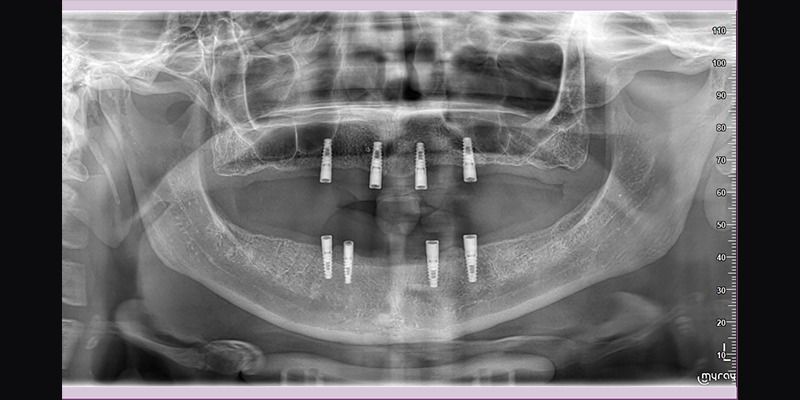
The patient had only 3 remaining maxillary teeth, which, upon initial intraoral examination, were found to be non-maintainable due to periodontal reasons. Additionally, tomographic analysis showed significant resorption in the width of the edentulous marginal crest.
It was decided to extract the remaining teeth and place four dental implants in the upper jaw, with simultaneous guided bone regeneration during surgery, followed by the placement of a removable overdenture on Locator abutments.
Surgical Phase
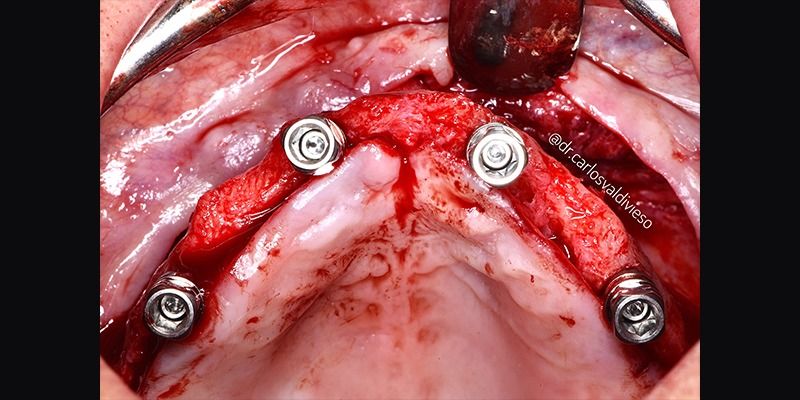
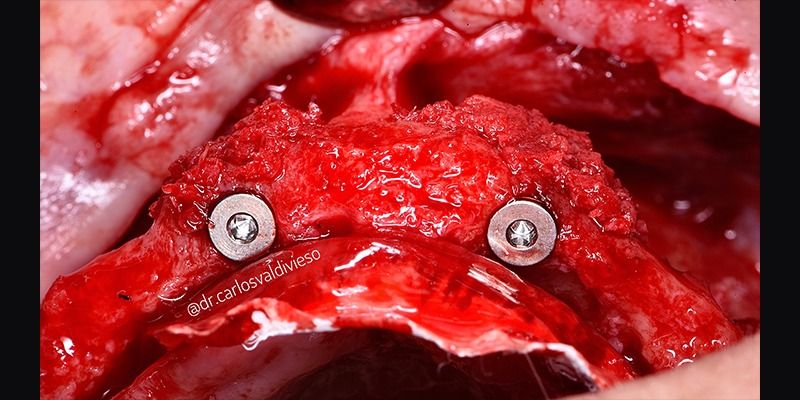
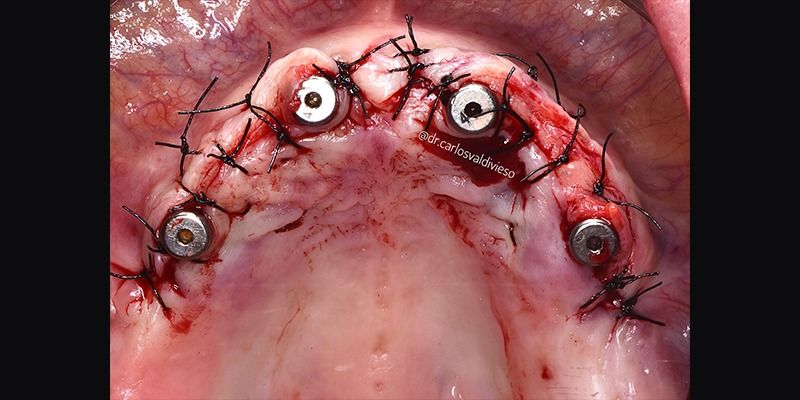
The patient was anesthetized, and a flap was raised from the area of the molars in the first quadrant to the molars in the second quadrant to place four Avinent Biomimetic Ocean IC implants with a diameter of 3.5mm and a length of 10mm in positions 12, 15, 22, and 24.
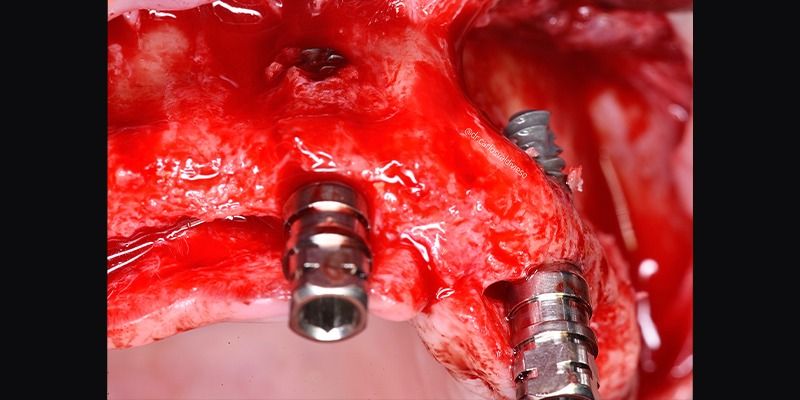
Due to the anatomy of the maxilla and the prosthetically guided placement of the implants, the two anterior implants fenestrated apically, leaving the apical half of the implant in position 22 and the apical third of implant 12 outside the bone.
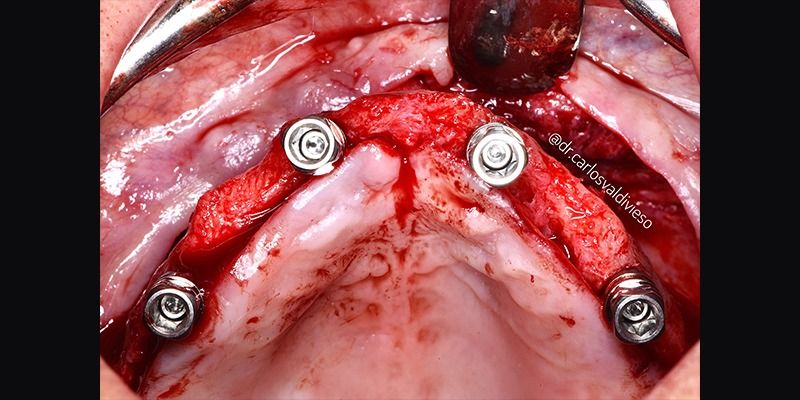
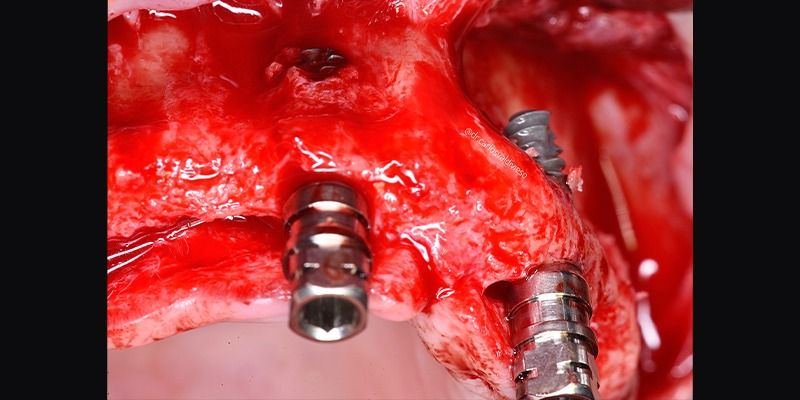

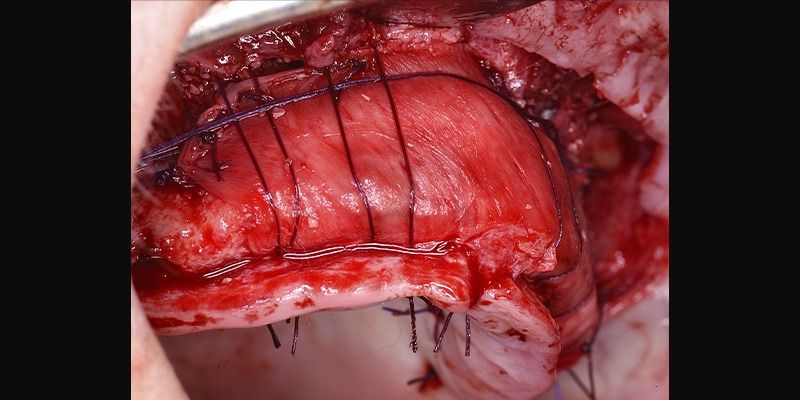
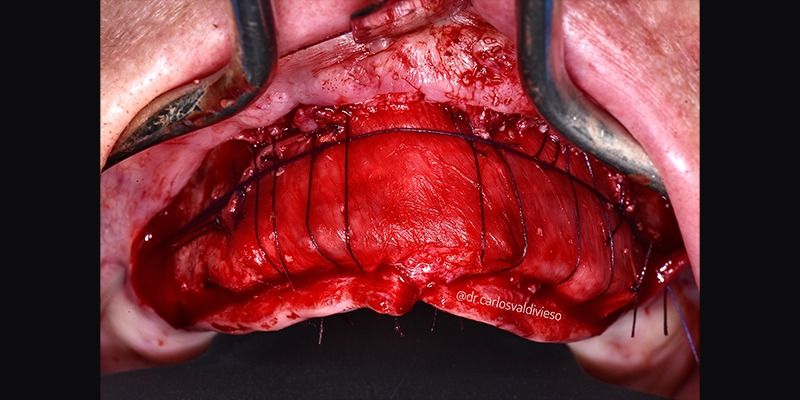
Once the implants were placed, guided bone regeneration was performed using a layered technique, where the first layer consisted of autologous bone obtained during the biological drilling of the implant beds, at low speeds and without irrigation, and the second outer layer consisted of xenograft (Genoss, Osteogenos). The entire regeneration was covered with a resorbable collagen membrane (Evolution STD, Osteogenos), securing the membrane with absorbable PGA suture to the periosteum to avoid a later re-entry to remove fixation elements.
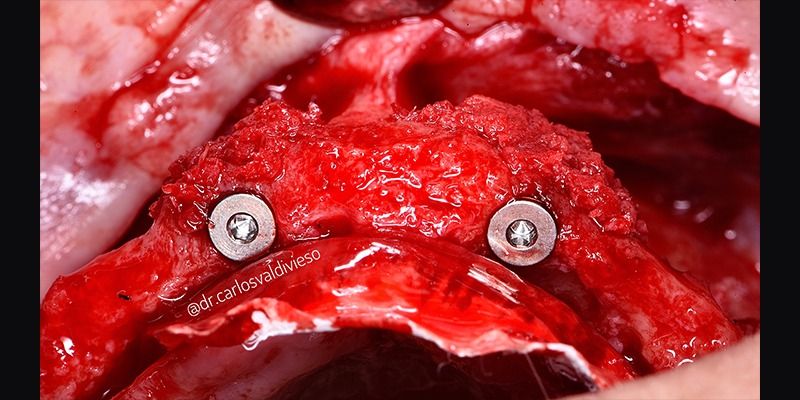

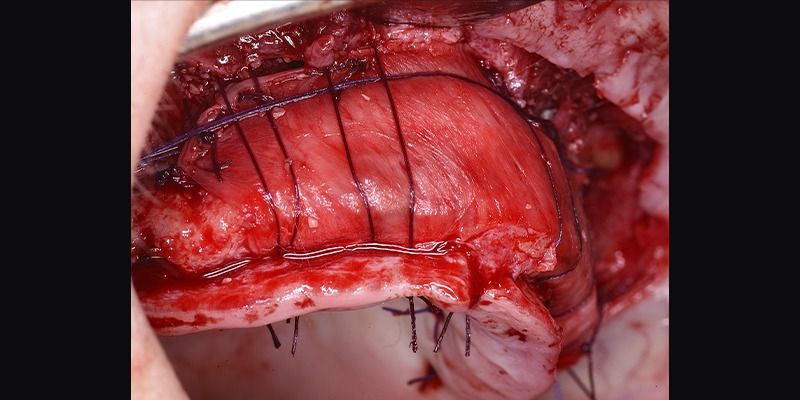
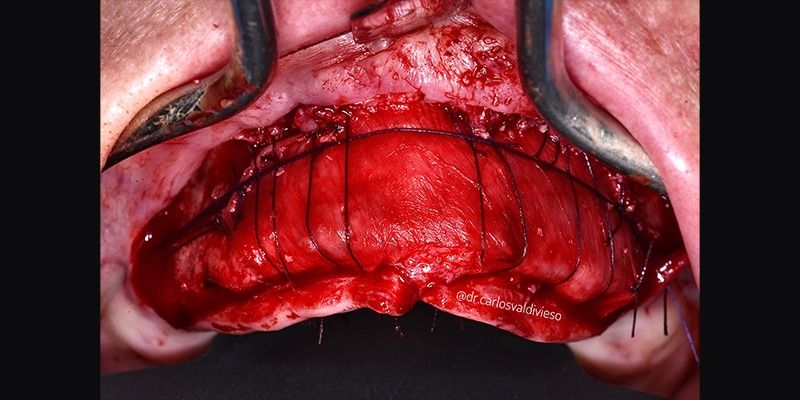
The success of GBR depends on four fundamental principles achieved during surgery and the healing period: good primary closure, angiogenesis, maintenance of space, and stability in the regeneration area.
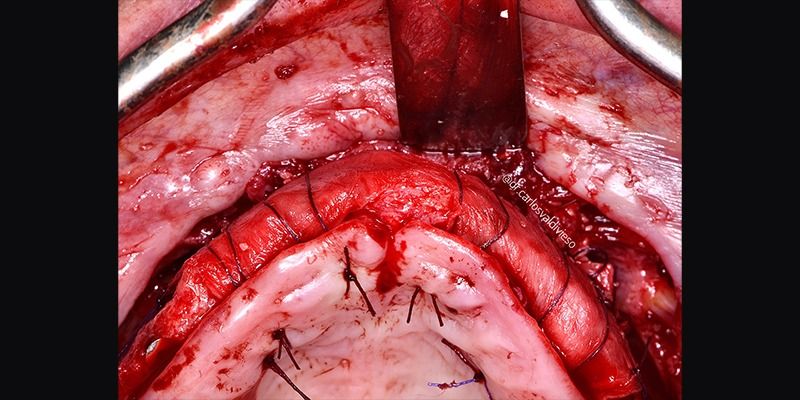
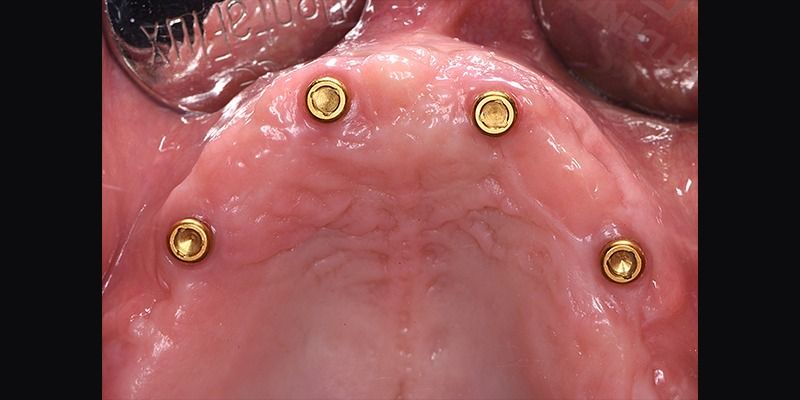
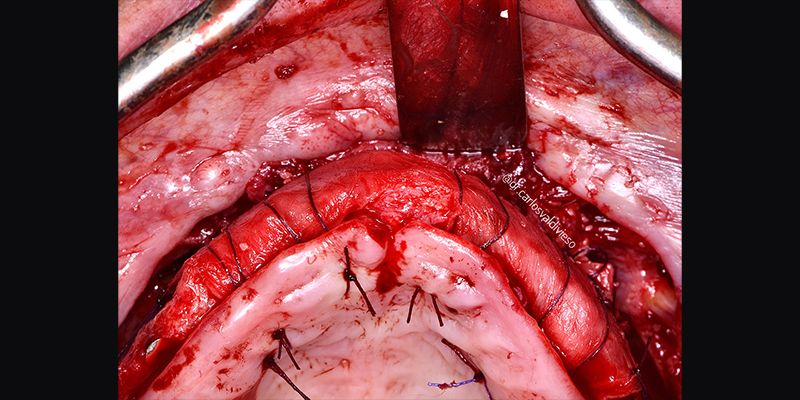
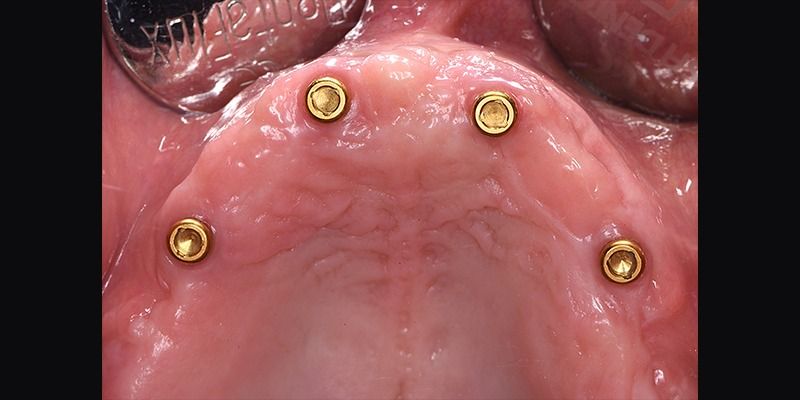
Following an uneventful postoperative period, healing abutments were placed in a second surgical stage after 6 months. At this same time, a periodontal "Roll Technique" surgery was performed to increase the amount of keratinized gingiva around the emergence of the implants, as significant regenerations can lead to a coronal migration of the mucogingival line and loss of attached gingiva. During this surgery, the closure plugs of the implants were replaced with healing abutments.
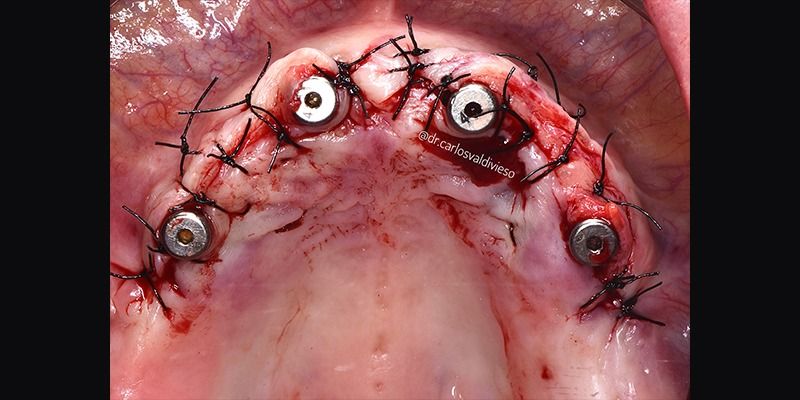
After six months of implant placement, observing proper healing and maturation of the soft tissues, impressions were taken for the fabrication of the definitive implant-supported removable prosthesis.



Conclusions
Inadequate bone volume can pose a challenge for the correct placement of implants for subsequent prosthetic rehabilitation. Therefore, simultaneous bone regeneration treatments may be required during implant placement, as these techniques are predictable for defects such as dehiscences and fenestrations.
Improving the environment of the peri-implant soft tissue, both for aesthetic purposes and to facilitate proper maintenance, is a common practice to achieve better predictability in implant treatments.