Introduction
Although the number of complete edentulous patients has decreased, there is still a group of patients who request treatment after the loss of their remaining teeth due to advanced periodontitis. In these cases, severe associated bone atrophy can be found, which makes conventional implant treatment difficult.
In order to be treated, these patients will require guided bone regenerative treatments prior or simultaneous to implant placement to augment the alveolar ridges and thus improve the long-term prognosis of the treatment.
As shown below, in this clinical case, current guided bone regeneration (GBR) techniques are an excellent guided bone regeneration (GBR) techniques are an excellent alternative for obtaining satisfactory aesthetic for obtaining satisfactory esthetic results in the regeneration of peri-implant defects.
Case presentation and planning
A 60-year-old female patient, ex-smoker and with no medical history of interest, came to the
of interest, came to the office to replace her removable partial prosthesis with a fixed rehabilitation.
The patient had only 3 maxillary teeth remaining in the mouth.
in the mouth, which in the initial intraoral examination were not maintainable due to
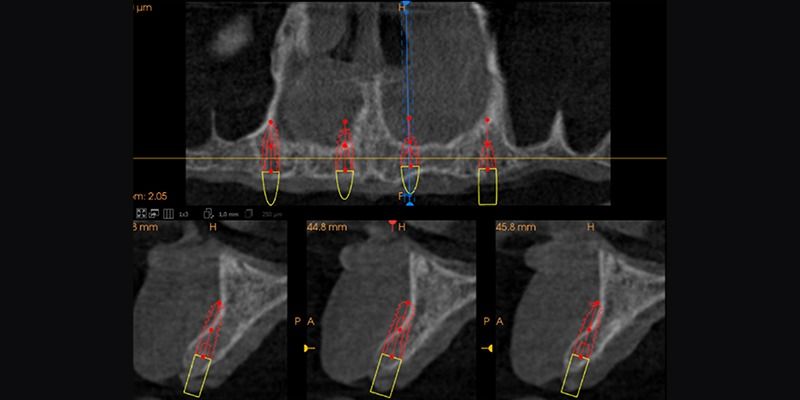
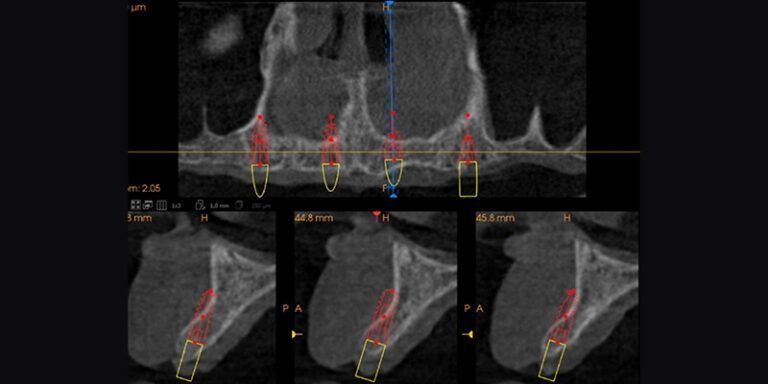
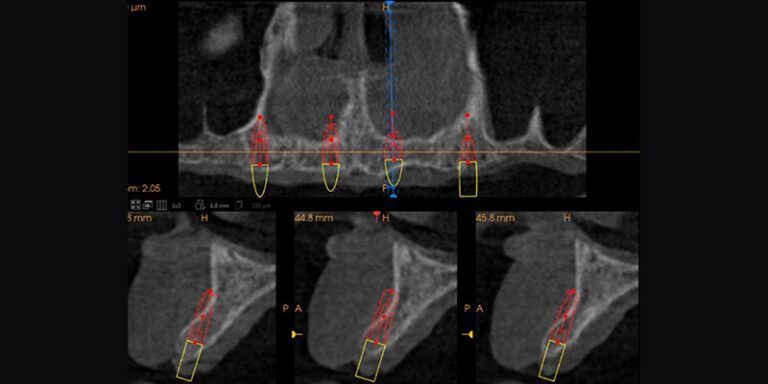
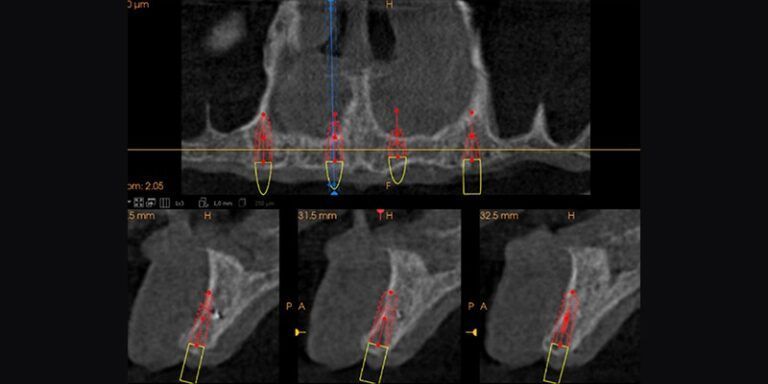
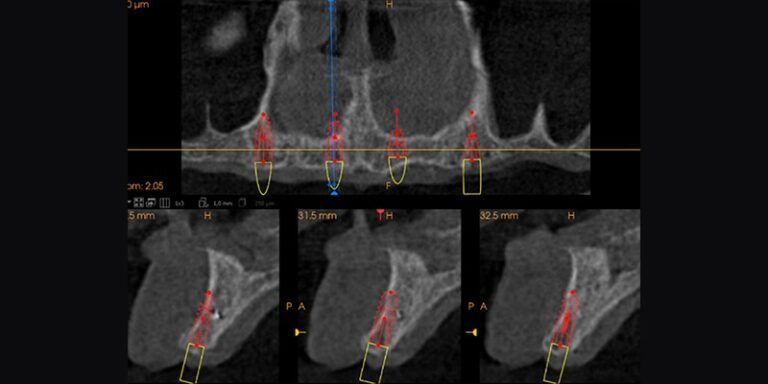
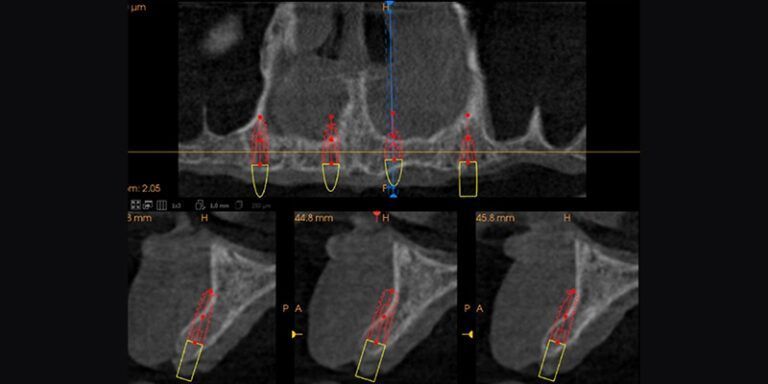
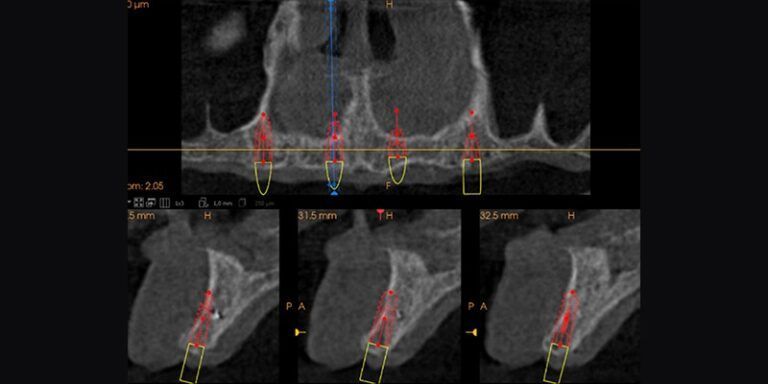
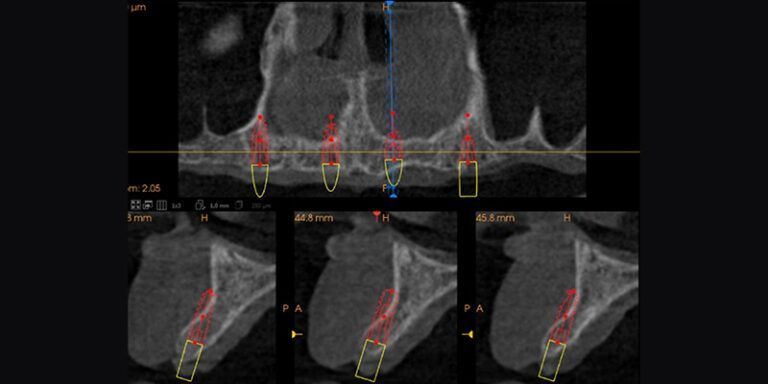
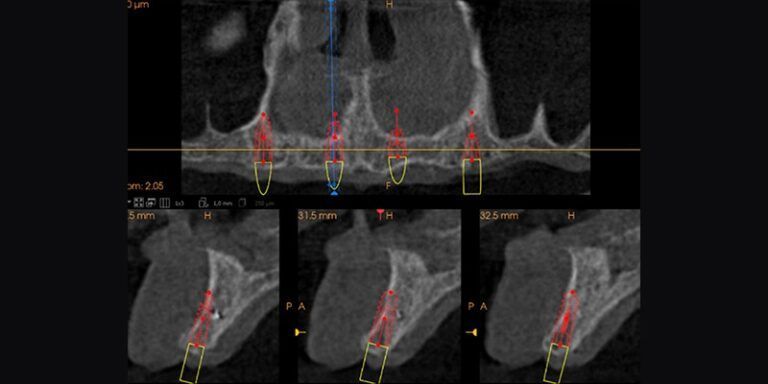
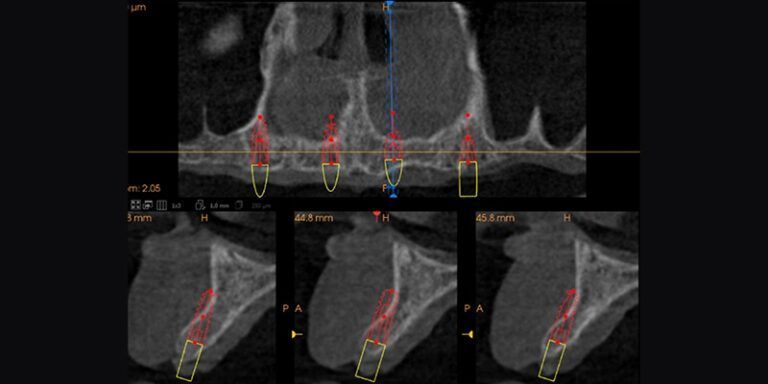
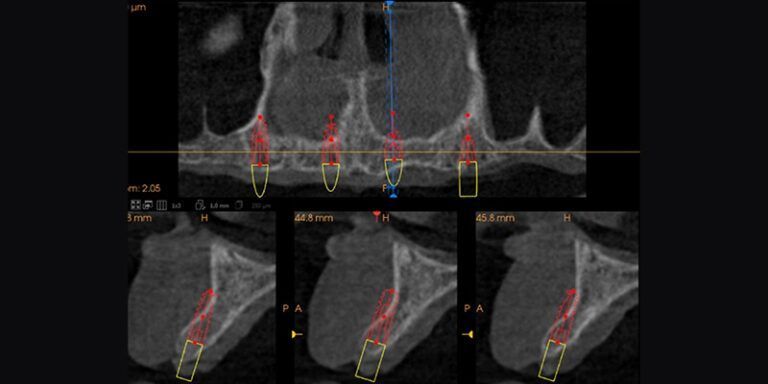
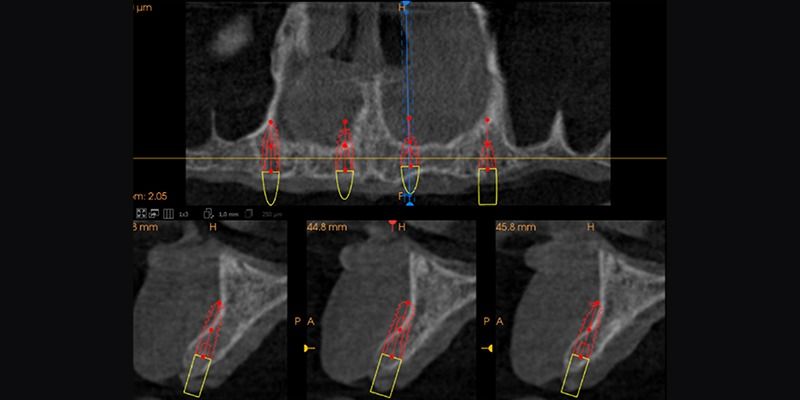
periodontal reasons. In addition, on tomographic analysis, a high level of resorption in
width resorption of the edentulous marginal ridge.
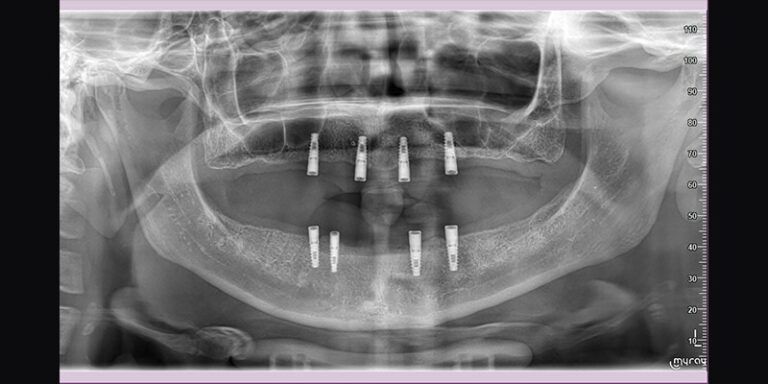
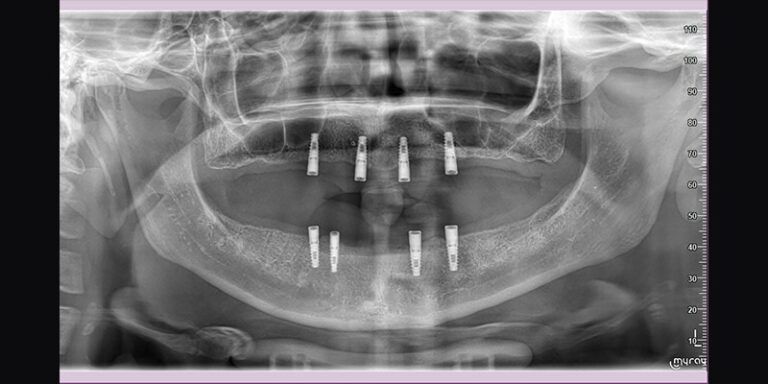
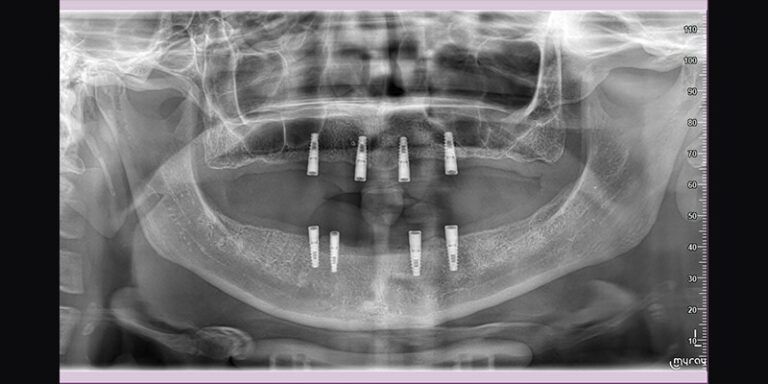
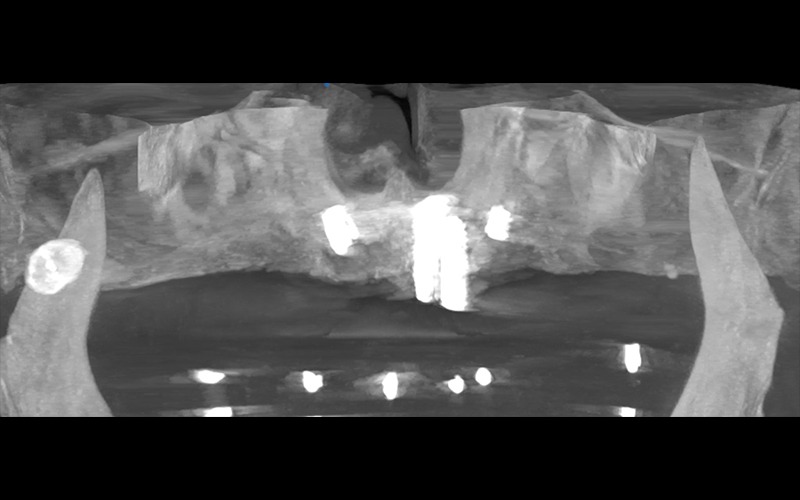
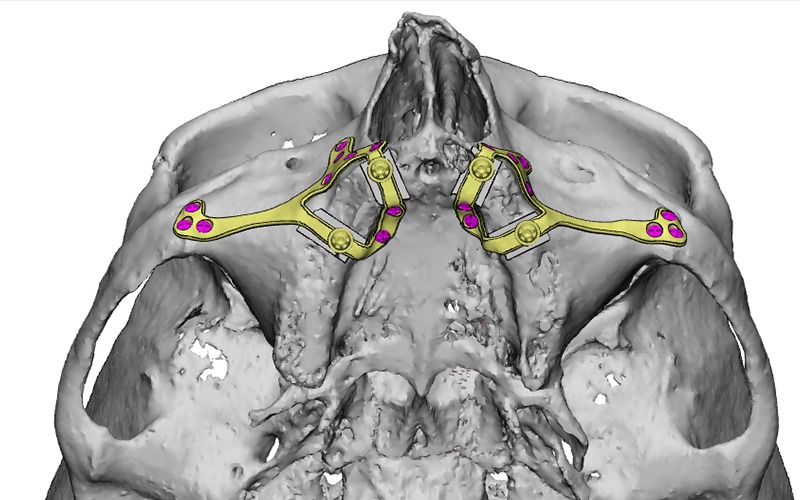
It was planned to extract the remaining teeth and place four dental implants in the upper jaw, with guided bone regeneration at the same time as the surgery, and the subsequent placement of a removable overdenture on Locator abutments.
Surgical phase
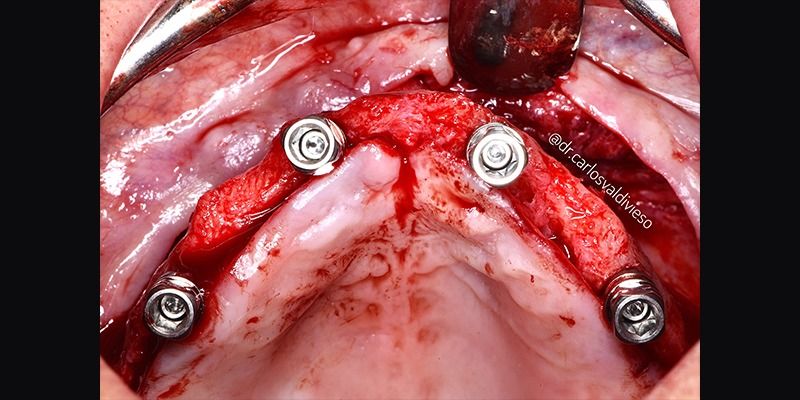
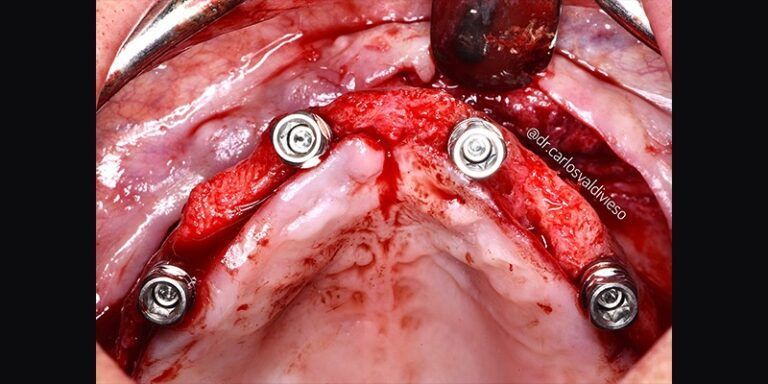
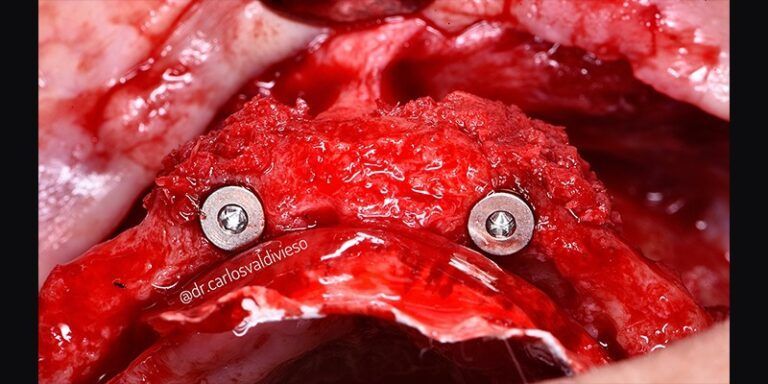
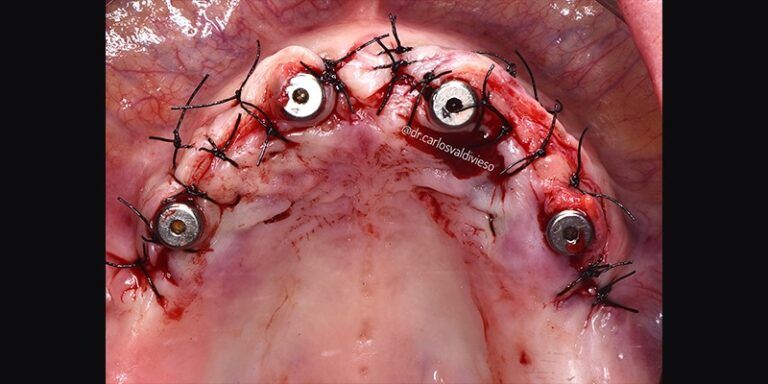
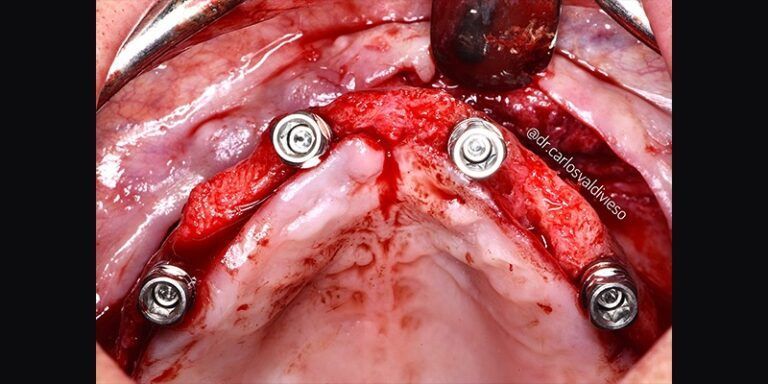
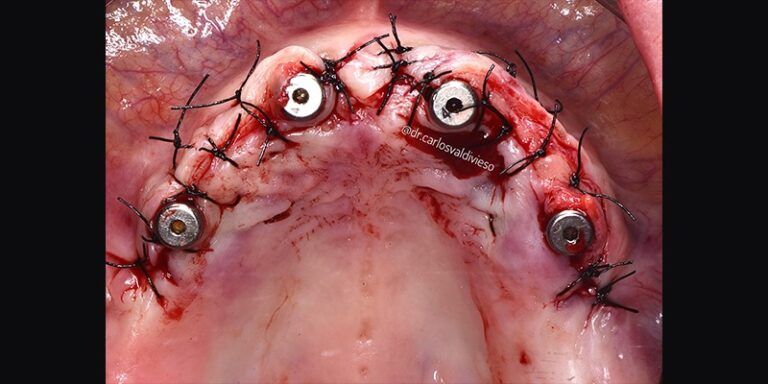
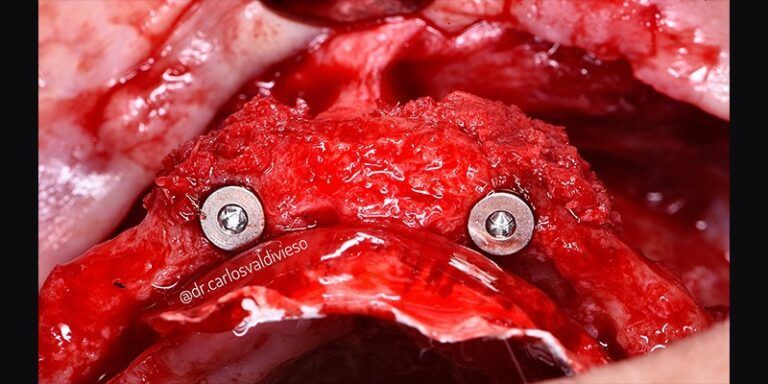
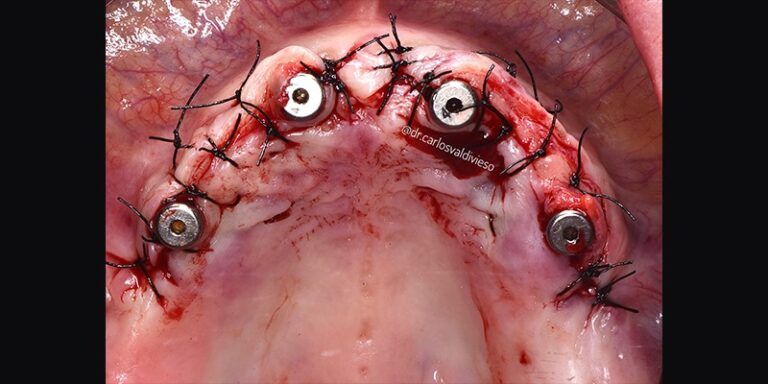
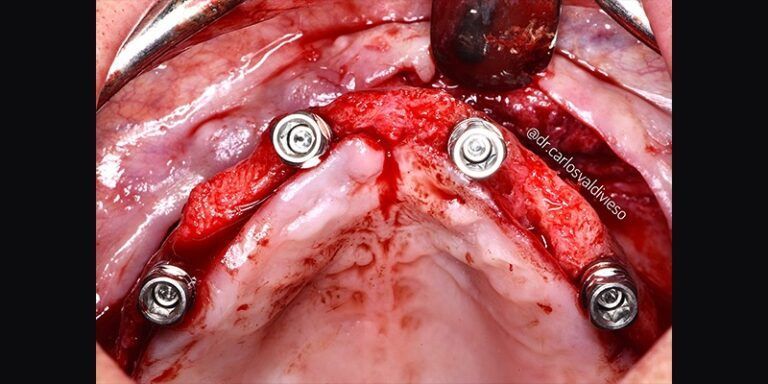
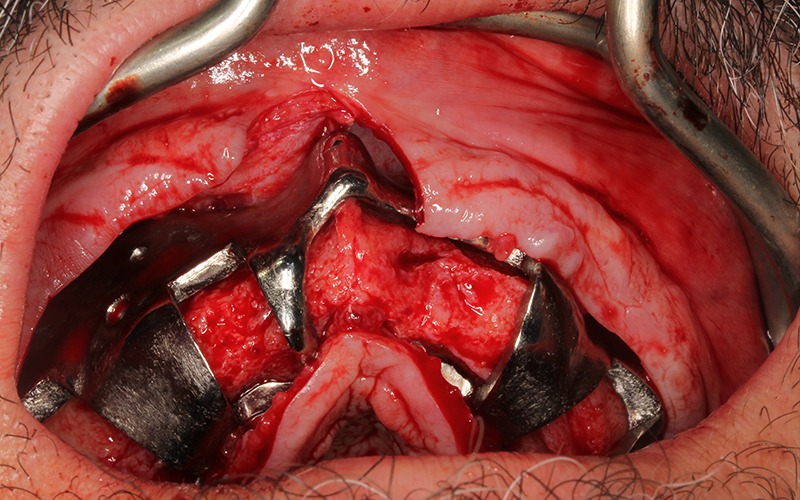
The patient was anesthetized and a flap was made from the molars of the first quadrant to the molars of the second quadrant to place four Avinent Biomimetic Ocean IC implants of 3.5mm diameter and 10mm in length in positions 12, 15, 22 and 24.
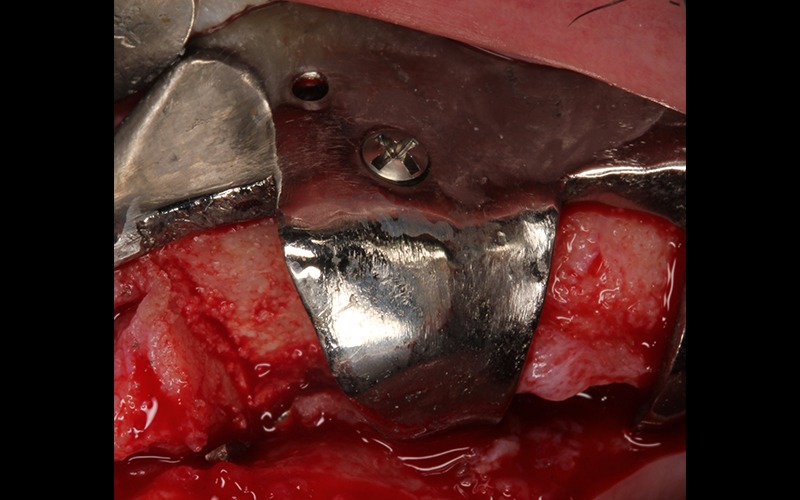
Due to the anatomy of the maxilla and the prosthetically guided placement of the implants, the two anterior implants were apically fenestrated, leaving the apical half of the implant in position 22 and the apical third of 12 outside the bone.



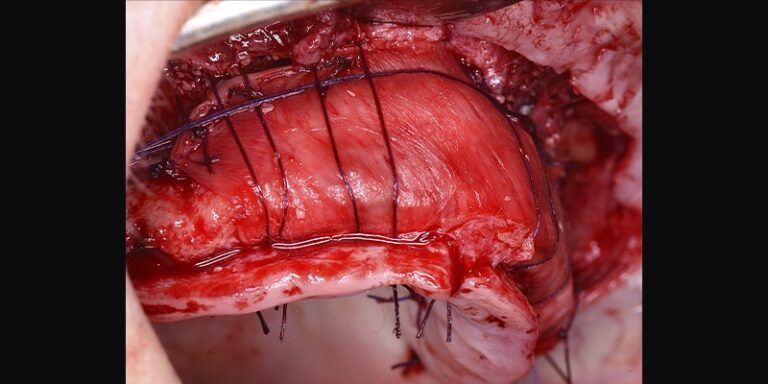
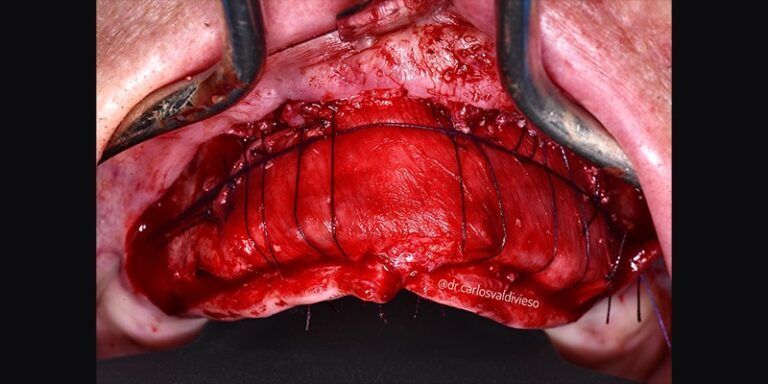
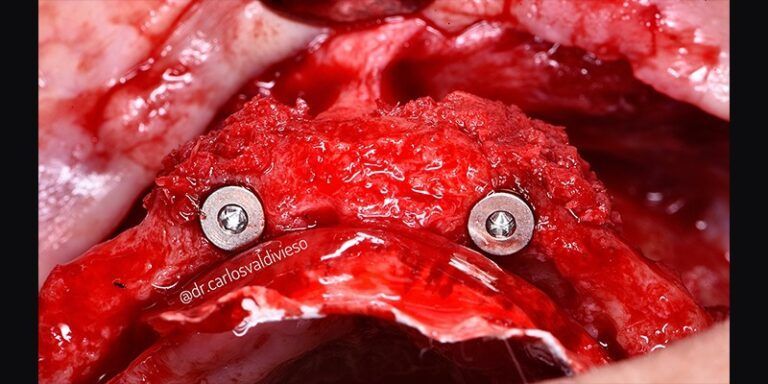
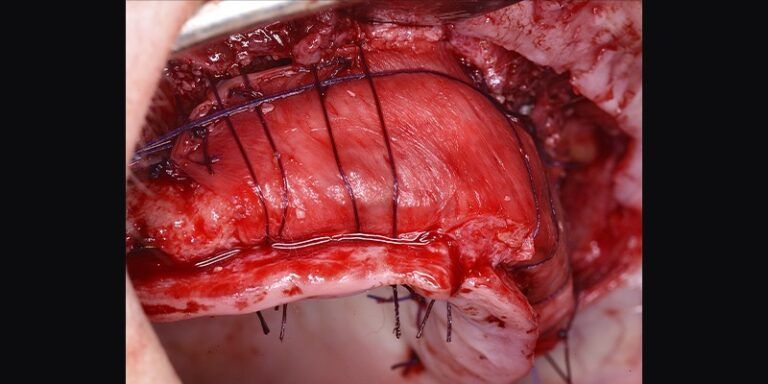
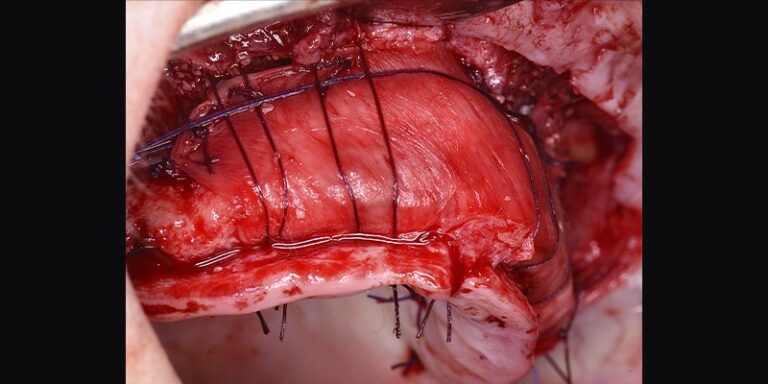
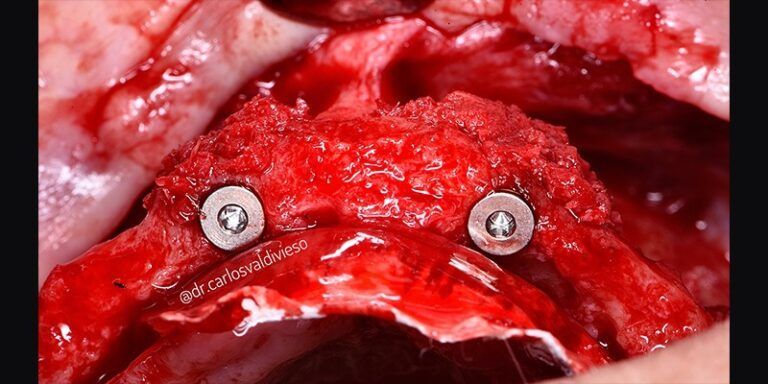
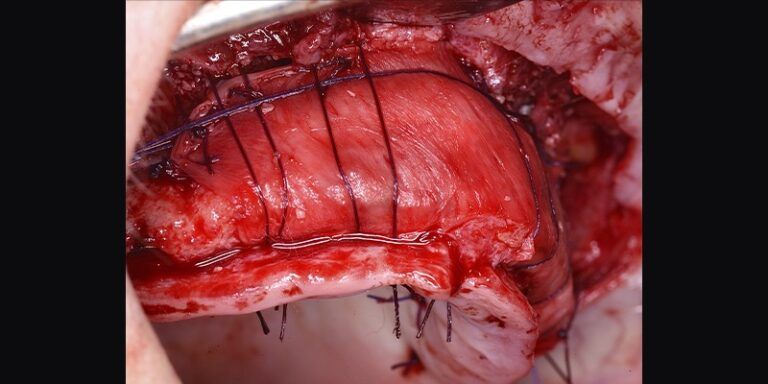
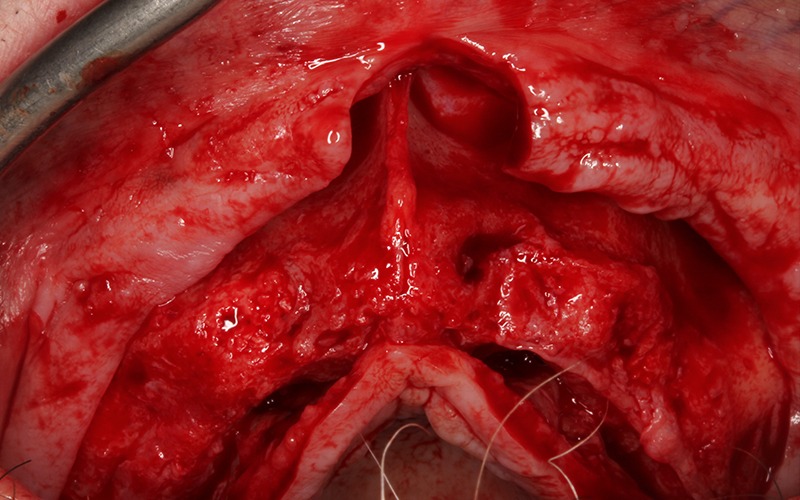
Once the implants were placed, guided bone regeneration was performed using a stratified technique, where the first layer was autologous bone obtained during the biological milling of the implant beds, at low revolutions and without irrigation, and the second, outermost layer of xenograft (Genoss, Osteogenos). The complete regeneration was covered with a resorbable collagen membrane (Evolution STD, Osteogenos), fixing the membrane with PGA resorbable suture to the periosteum to avoid subsequent re-entry to remove fixation elements.



The success of ROG is dependent on four fundamental principles
during surgery and the healing period: good primary closure, angiogenesis, space maintenance and stability of the regenerative zone.
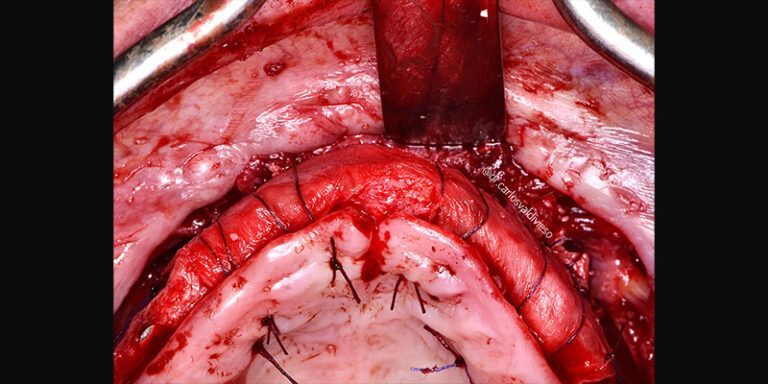
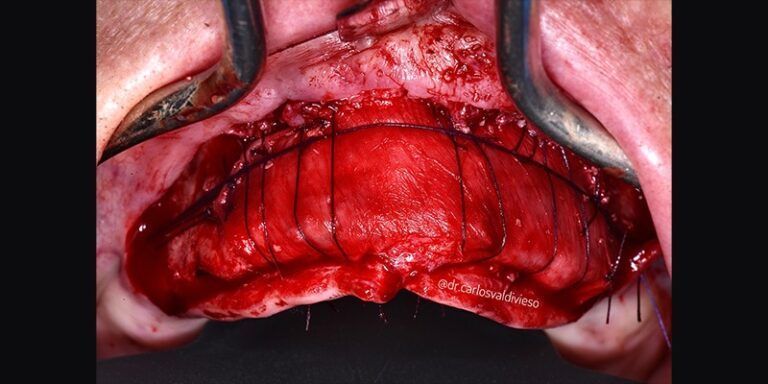
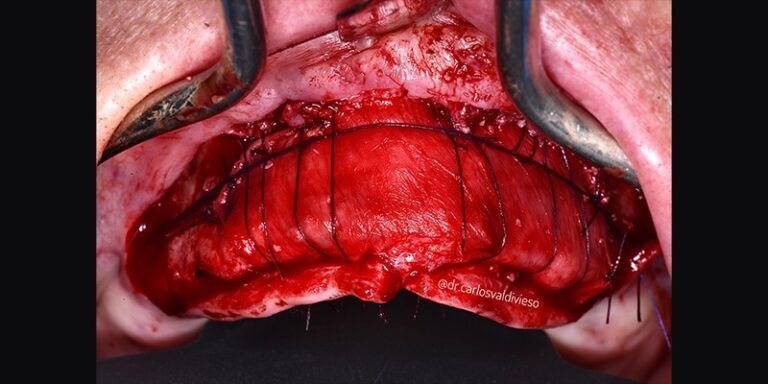
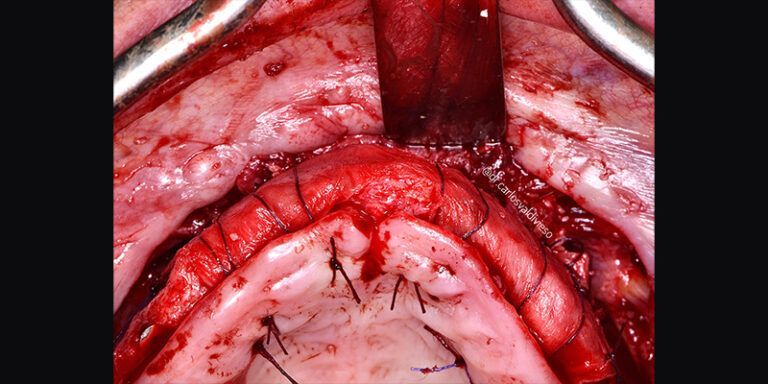
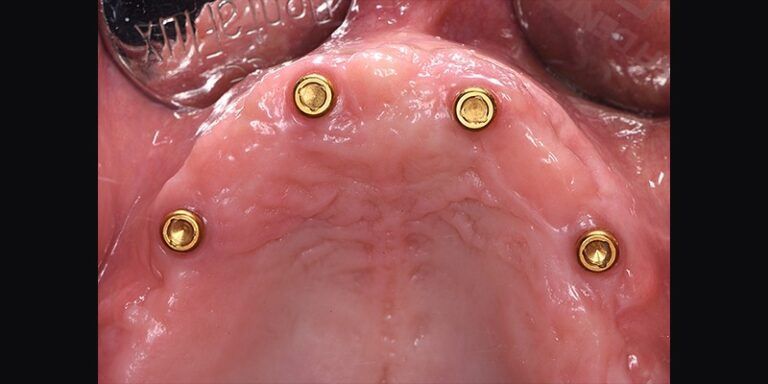
After an uncomplicated postoperative period, healing abutments were placed in a second surgical stage at 6 months. At the same time, periodontal “Roll Tecnique” surgery was performed to increase the amount of keratinized gingiva around the emergence of the implants, since, in cases of large regenerations, there is a coronal migration of the mucogingival line and adherent gingiva is lost. In this same surgery, the closing plugs of the implants were replaced by healing abutments.

Six months after implant placement, and observing correct healing and maturation of the soft tissues, impressions were taken for the fabrication of the definitive implant-supported removable prosthesis.



Conclusions
Inadequate bone volume can pose a challenge for the correct placement of implants for subsequent prosthetic rehabilitation.
This is why bone regeneration treatments simultaneous to implant placement are sometimes required, considering them as predictable techniques in defects such as dehiscence and fenestrations.
Improving the peri-implant soft tissue environment, both for esthetic purposes and to facilitate proper for esthetic purposes as well as to facilitate proper maintenance, is a common practice for better predictability of implant treatments.