Introduction
The use of osseointegrated implants to replace natural teeth that have been lost is widely documented on a scientific level and today constitutes a predictable long-term therapeutic option in different clinical situations.
Risk factors such as smoking or a history of periodontitis of the patient, together with poor oral hygiene, can lead to the loss of the dental implants and, therefore, the failure of the implant treatment. Bone regeneration.
For a satisfactory long-term prognosis of dental implants, one of the main factors to take into account is the maintenance or improvement of the quality and stability of the soft tissue-implant interface. For this purpose, the Biomimetic Iceberg implant presents a converging morphology at the transmucosal neck, with no angles or edges, that makes it possible to respect the biology of the periimplant tissues, ensuring the seal and facilitating the correct maintenance of the implant.
Case presentation
Male patient aged 64 years, with mild systemic disease ASA2, attended the clinic with pain, inflammation and odour in the anteroinferior area.
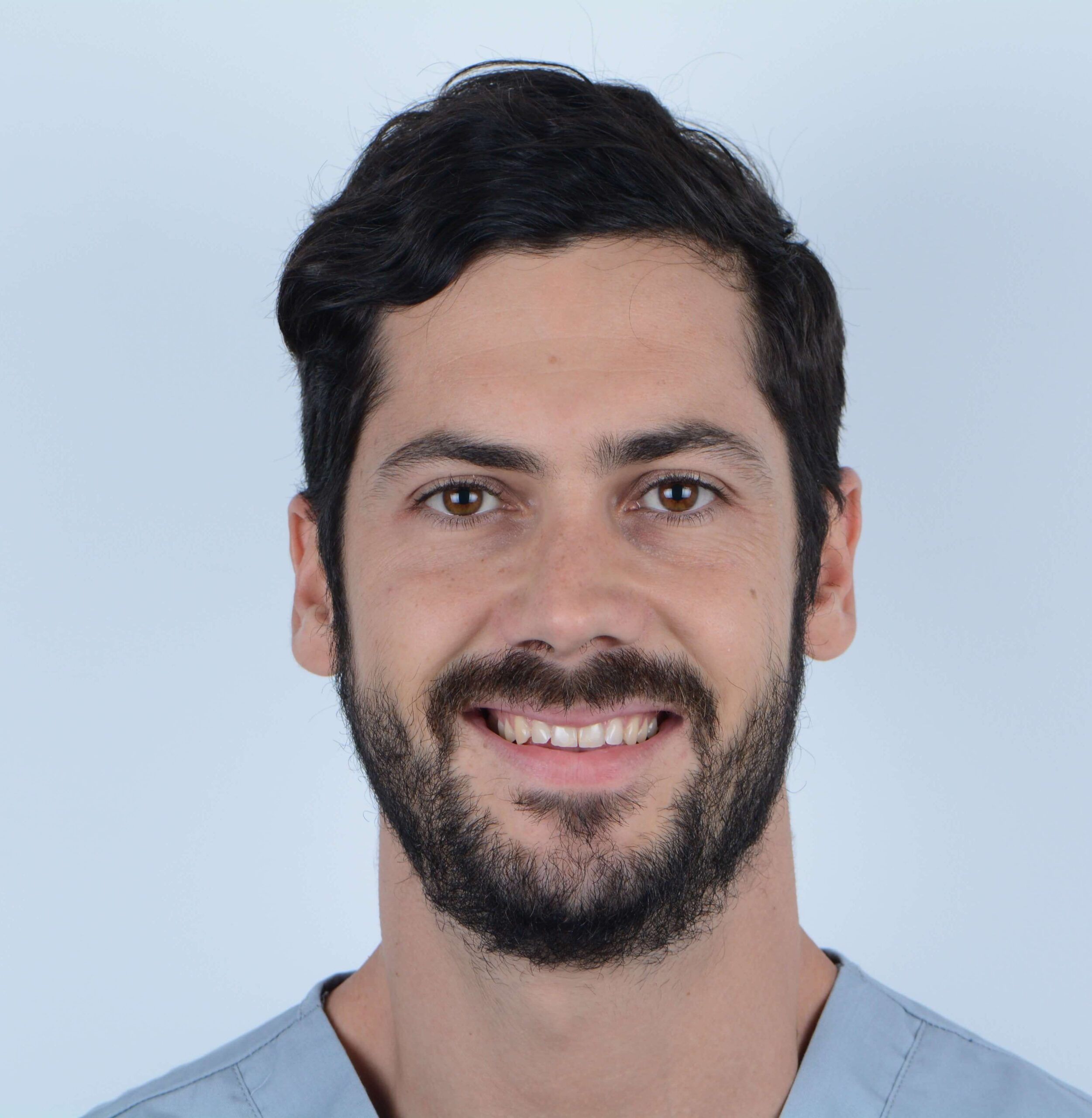
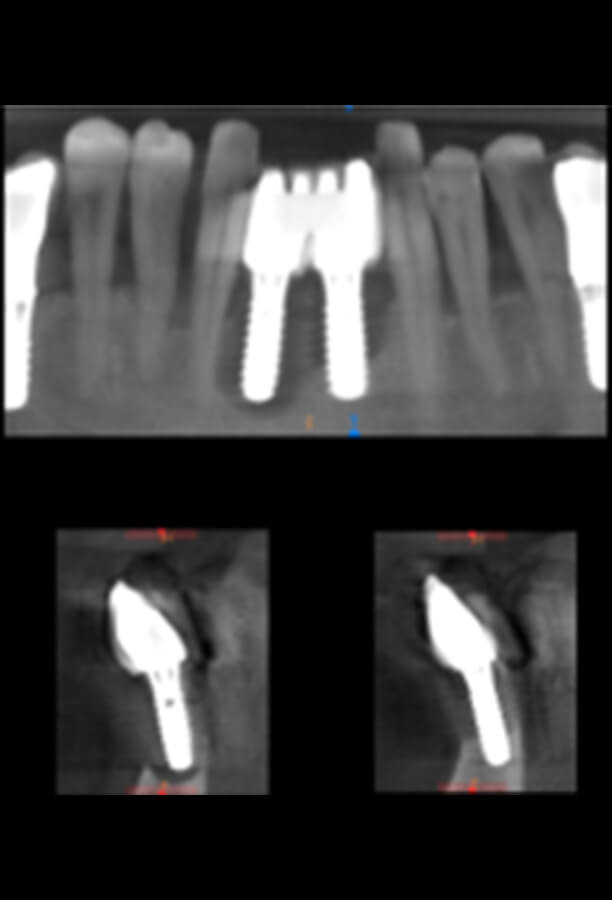
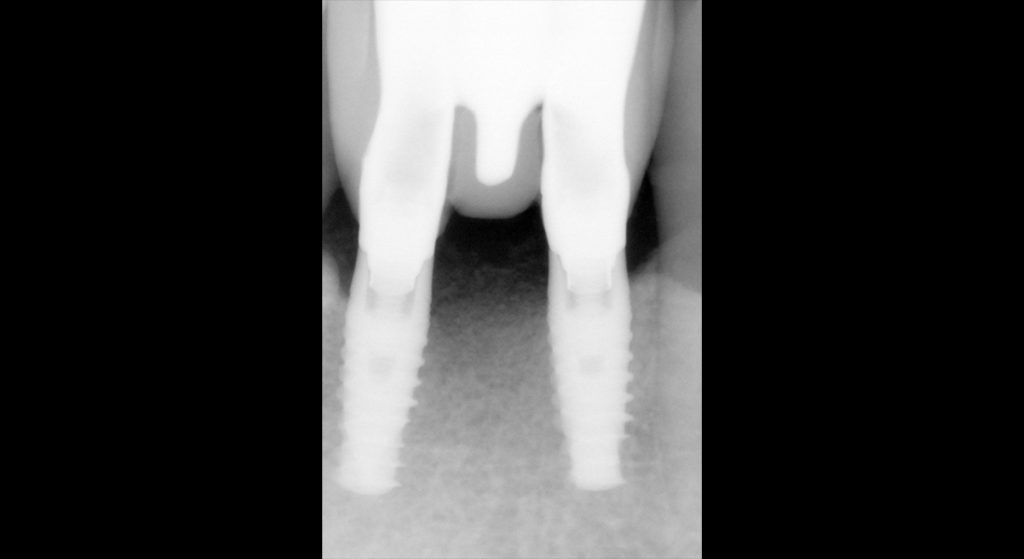
The patient is a smoker with poor hygiene, and no periodontal checks for years. The intraoral examination revealed an advanced degree of periodontitis, stage IV grade B, with periodontal destruction, presence of deep pockets and a significant intraosseous defect in the anterior area of the inferior maxilla where he had two implants.
Treatment
After an exhaustive evaluation of the case, it was concluded that in addition to periodontal treatment, complex multidisciplinary treatment was required.
We started with periodontal therapy, in this case non-surgical. Two sessions of scaling and root planing were carried out 5 days apart, combined with a systemic antibiotic treatment for 7 days and application of local chlorhexidine for 15 days.
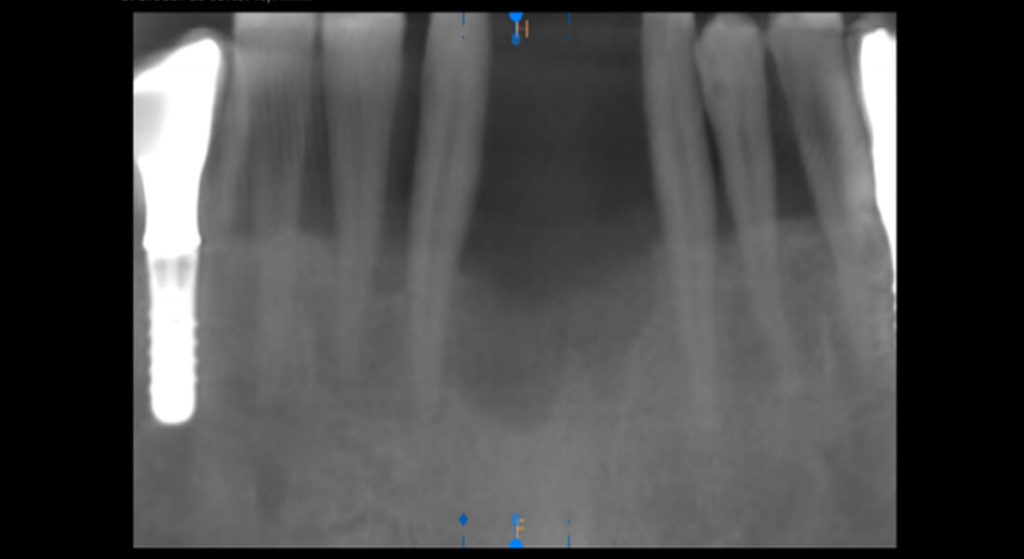
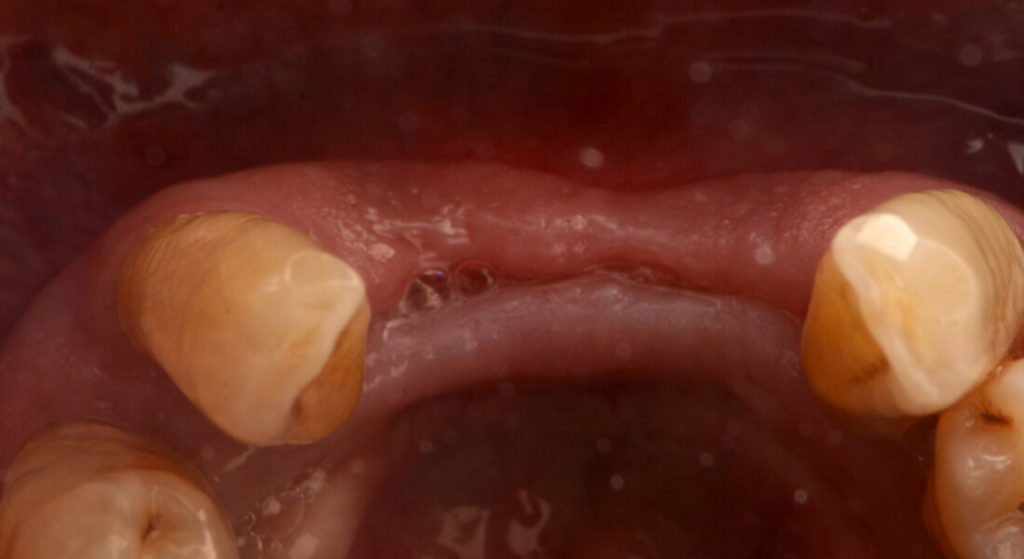
At the 5-week reevaluation the patient presented stabilization of the disease in all sites except in sextants 1 and 5. In sextant 1 pocket reduction surgery with a modified Widman flap was carried out, with good curettage of granulation tissue. The root cleaning was completed in the deepest areas and the bone architecture was modified to achieve a more favourable situation, compatible with periodontal health. Meanwhile, sextant 5 presented two implants affected by periimplantitis with an impossible prognosis.
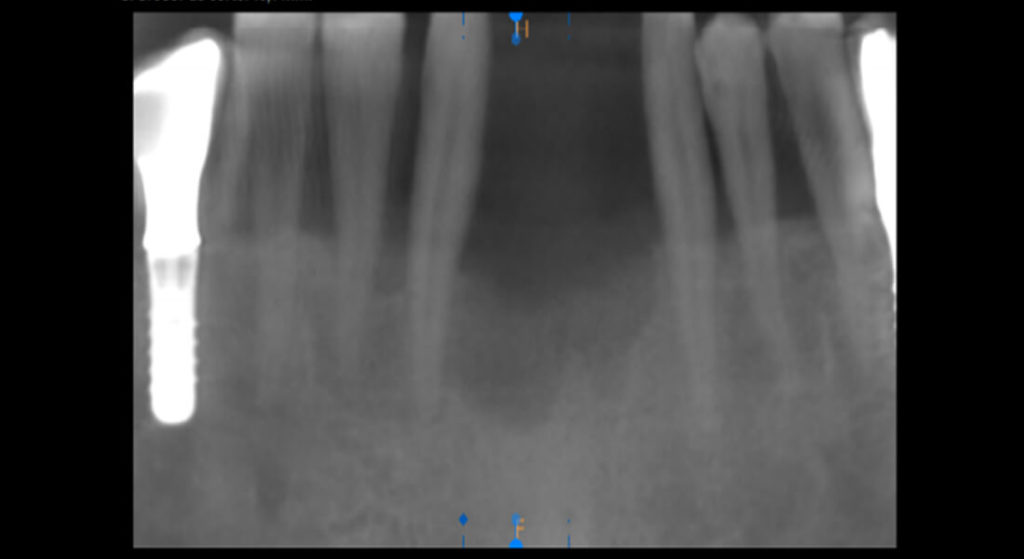
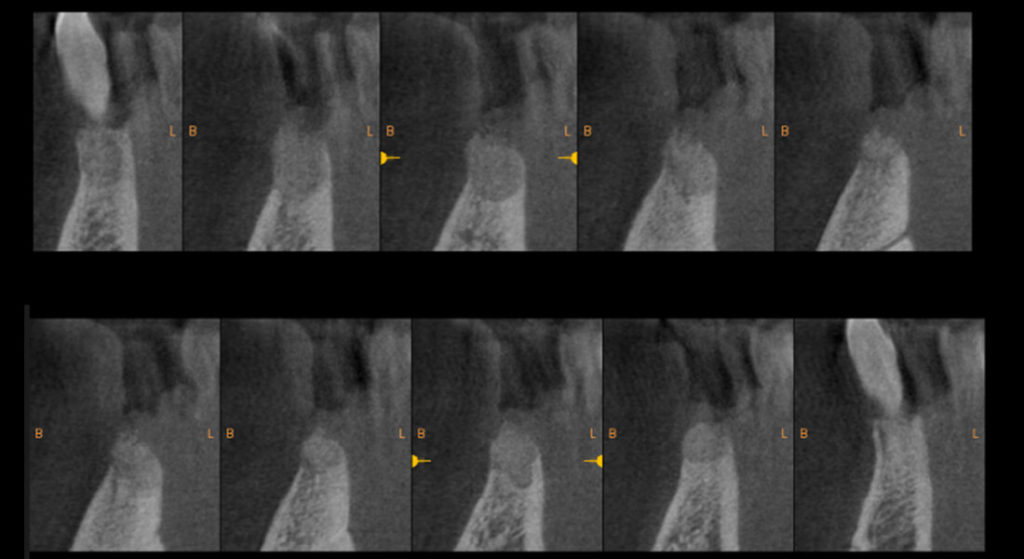
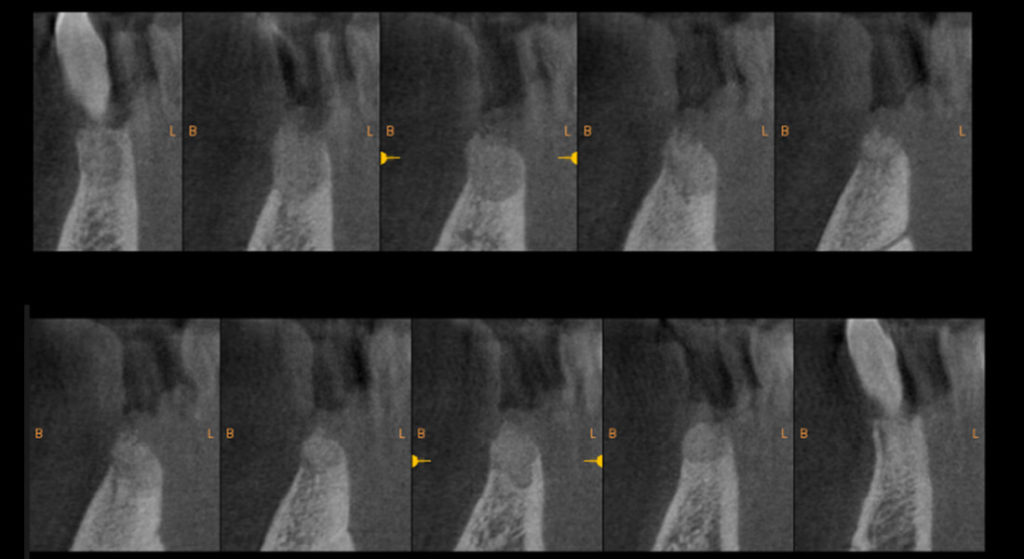
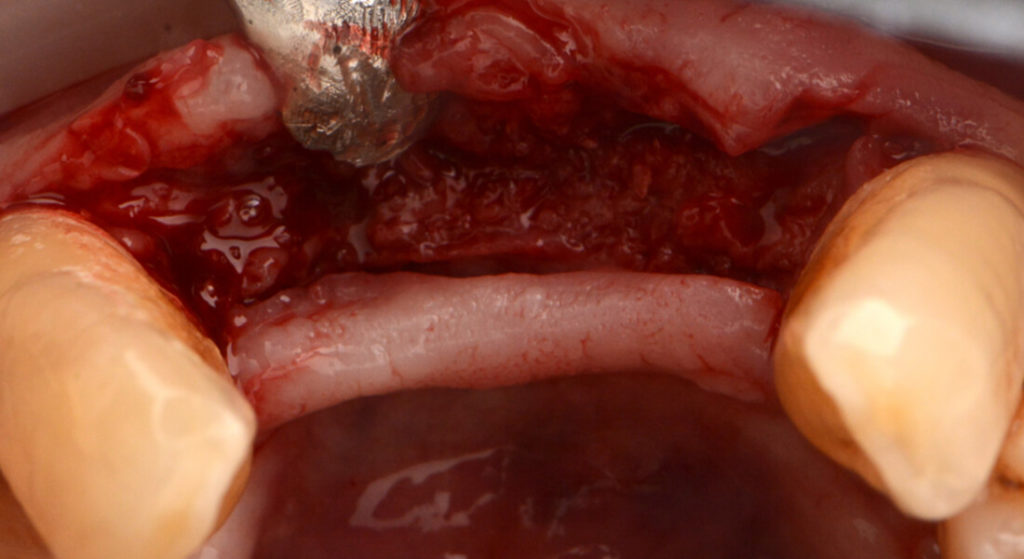
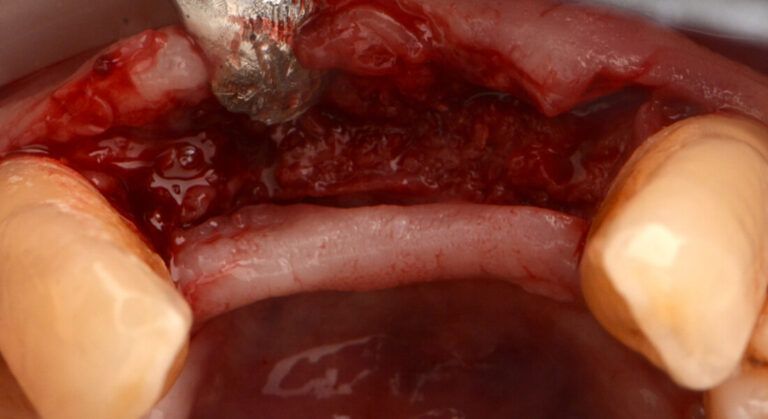
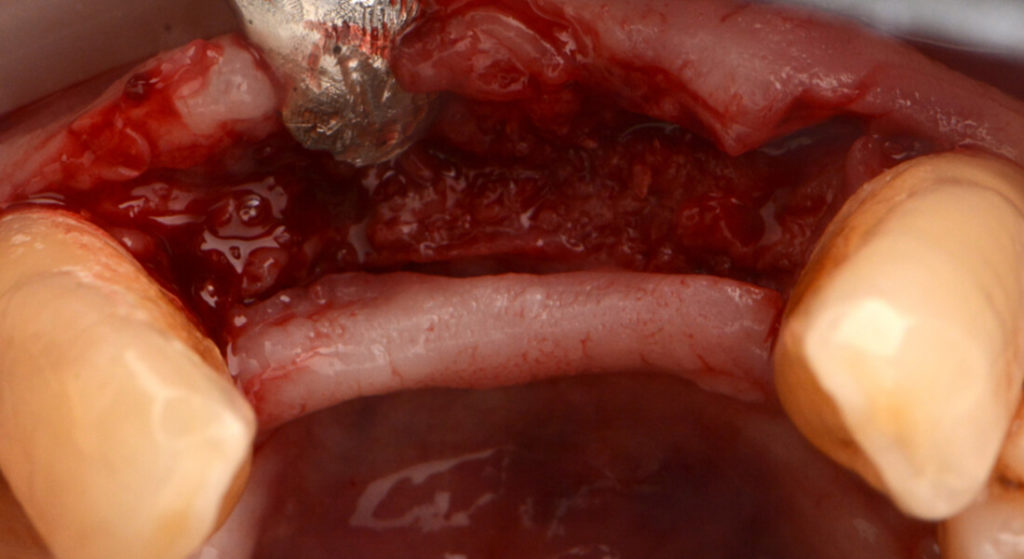
After extracting the two implants, and once the defect had been cleaned and prepared, guided bone regeneration with particulate bone and reabsorbable membrane was carried out due to the large resulting defect.
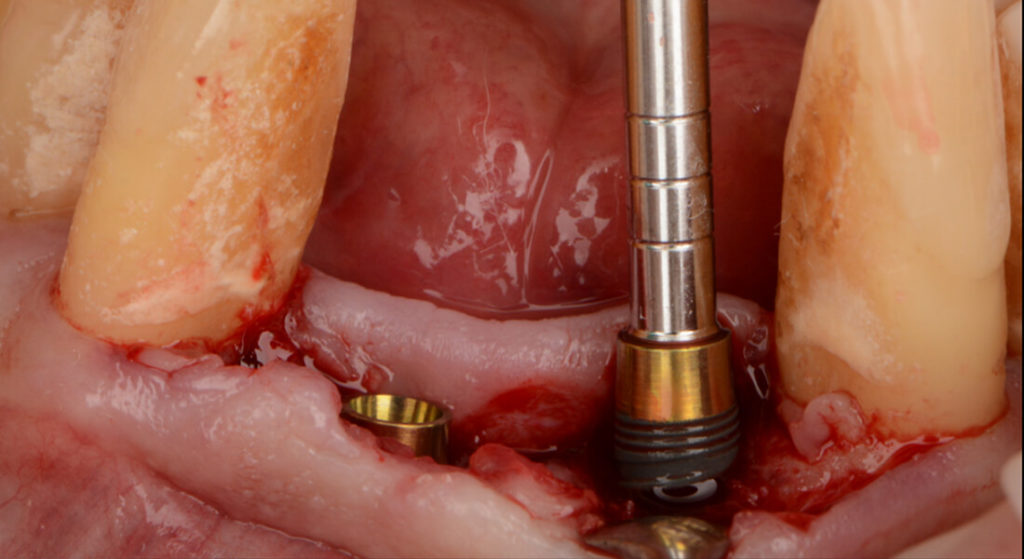
Image of the large defect after the extraction of the implants Details of regenerated bone after the GBR therapy Appearance of the tissues once the regenerated bone had healed Appearance of the tissues once the regenerated bone had healed
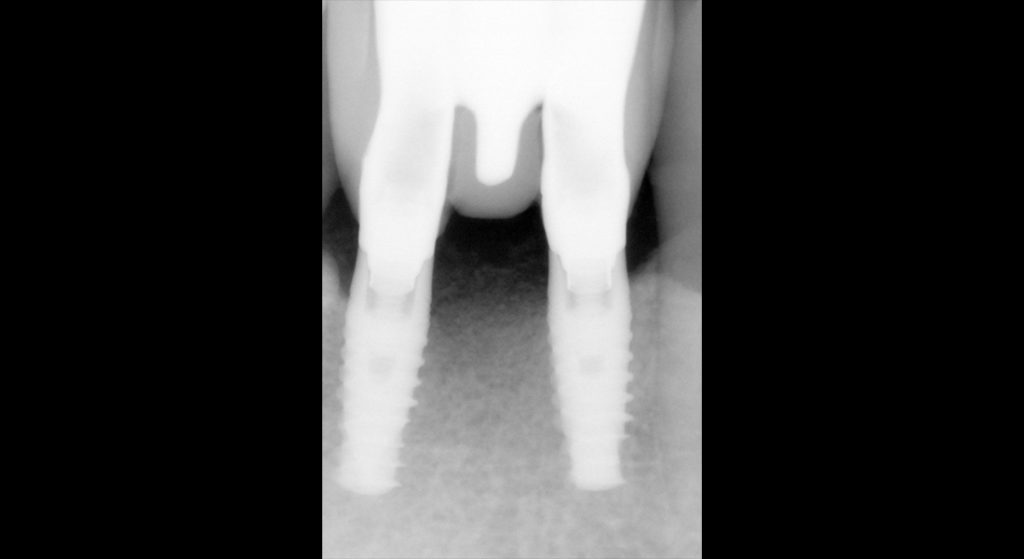
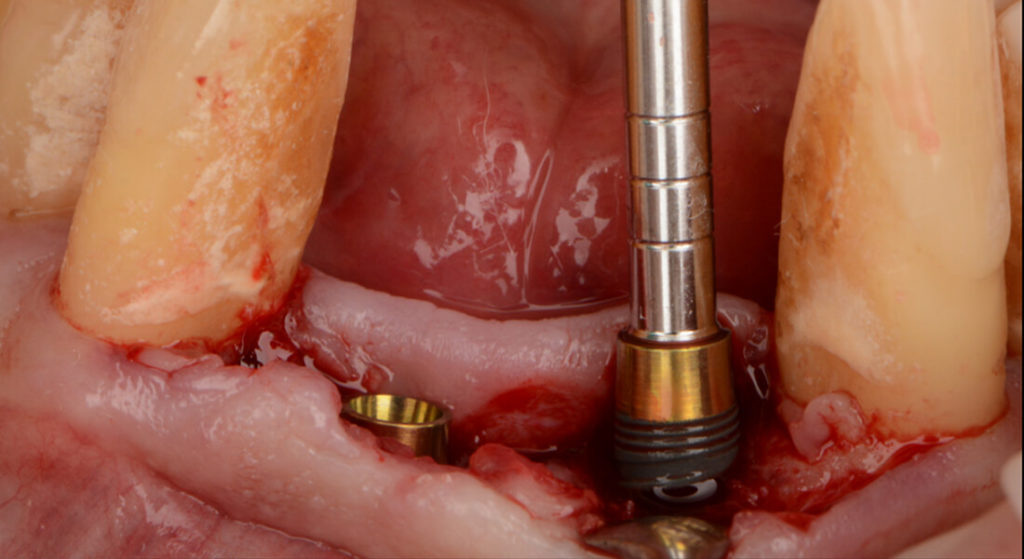
Six months after the bone regeneration, another incision was made observing the type II-III newly formed bone. A minimal flap was made to check the bone edge, without disbonding the periosteum excessively so as not to compromise the vascularization of this new regenerated bone.
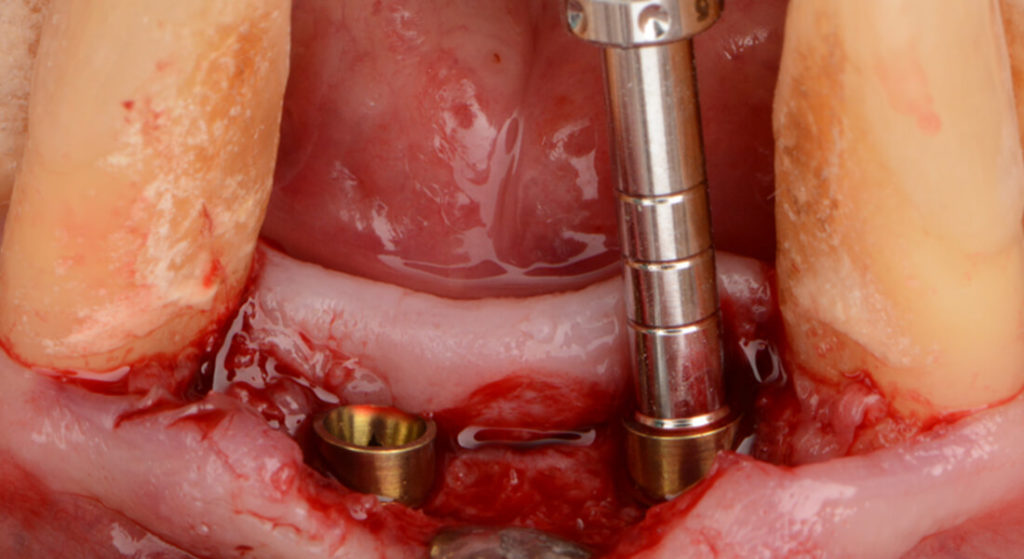
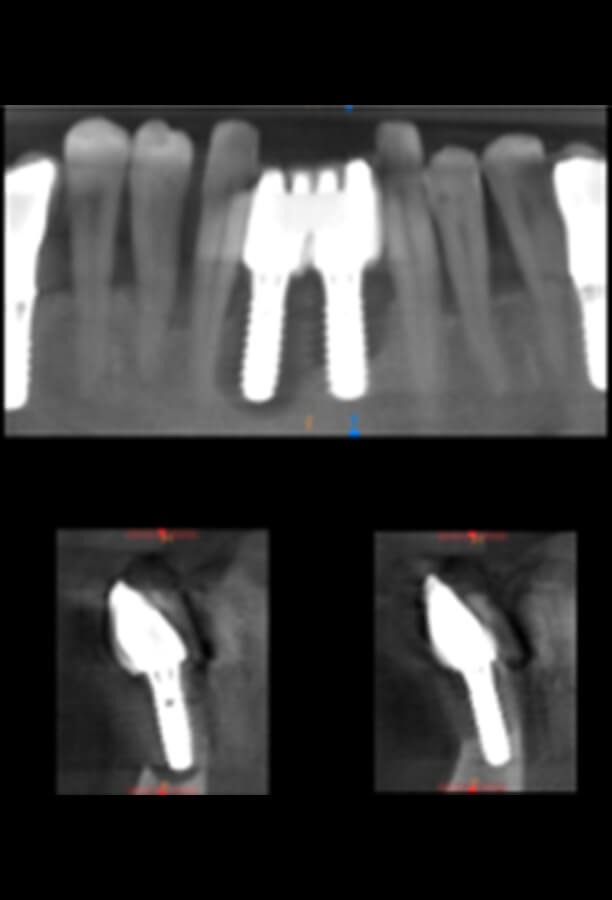
Two Biomimetic Iceberg dental implants by Avinent, 4 mm in diameter and 10 mm long, were placed in positions 32 and 42, with an insertion torque of approximately 35 Ncm for both implants.
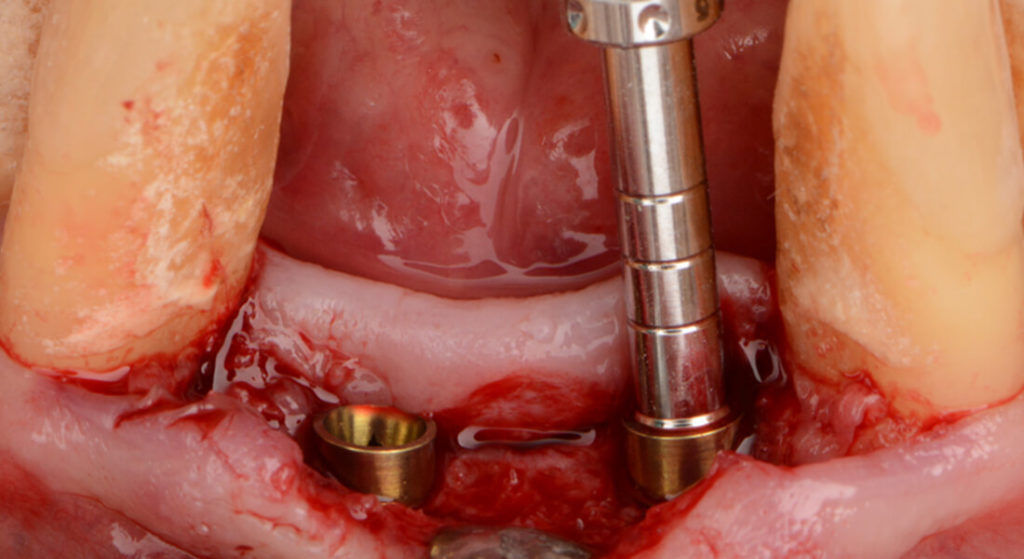
Biomimetic Iceberg Implant Placing the Biomimetic Iceberg implants View of the implants in place, with the polished collar at the transmucosal level
View of the implants in place, with the polished collar at the transmucosal level
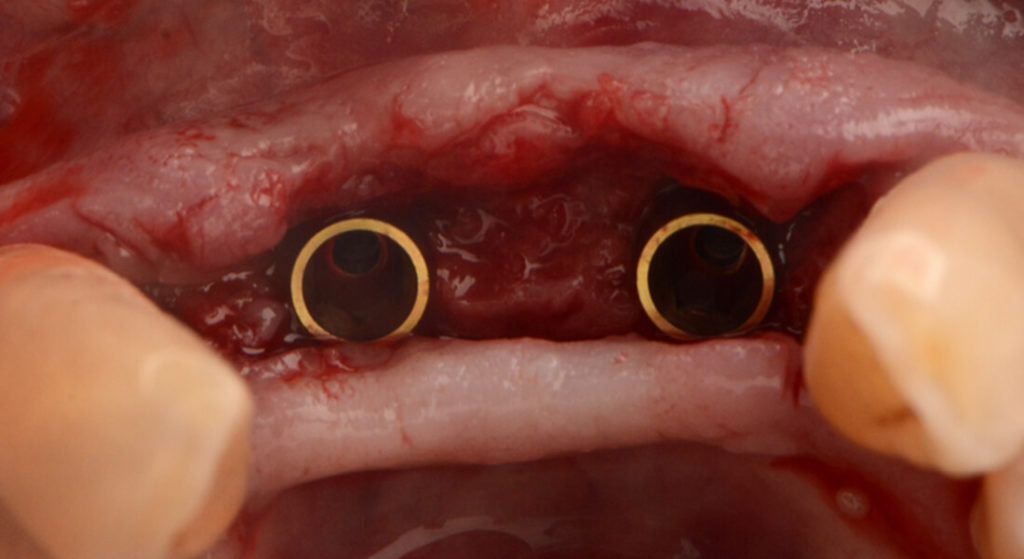
Due to the good primary stability achieved, healing abutments with a height of 3 mm were placed in the same surgery to avoid a second surgical intervention.
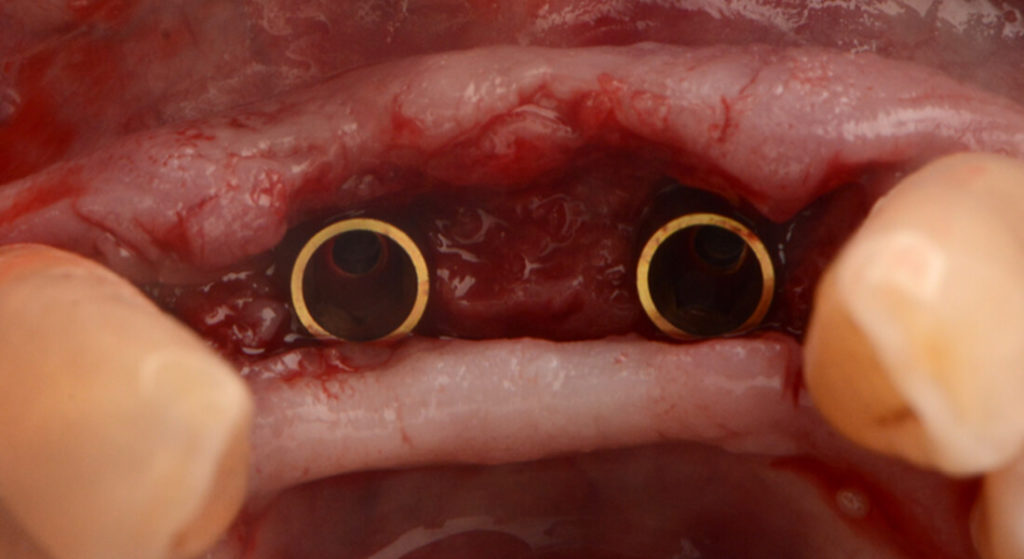
Anodized healing abutments Anodized healing abutments X-ray check of the fit of the healing abutments
Three months after implant placement, they were checked to ensure the symptoms had disappeared and that there was no recurrence of the periodontal disease. Impressions were taken to design and manufacture a multiple cemented-screw-mounted prostheses in zirconium on titanium bases.
Taking conventional impressions Definitive prosthesis in the mouth Definitive prosthesis in the mouth Details of the final zirconium prosthesis
Conclusion
In this case,
the periodontal treatment led to an improvement of the clinical periimplant
parameters that, along with the guided bone regeneration technique, made it
possible to achieve a favourable situation to then fit the dental implants in
the same area.
In patients
with high periodontal risk that need extreme care of the tissues and
periimplant health, the
design of the Biomimetic Iceberg implant is ideal. Its geometry
makes it possible to keep the implant-prosthesis connection away from the bone,
decreasing the risk of periimplant bone loss, and allowing the tissue to be
modelled thanks to the transmucosal collar with a converging profile and the
continuity of this design in the prosthetics line.
A year and
two months after restoring the case, and despite the patient’s poor hygiene and
smoking habit, the implants and their surrounding tissues remain in optimal
condition.
Details of the final prosthesis 1 year and 2 months after the restoration Details of the final prosthesis 1 year and 2 months after the restoration Details of the final prosthesis 1 year and 2 months after the restoration
The patient’s expectations were very much met; tissue health was recovered and the functional and aesthetic limitations of the anterior teeth were improved.
Initial situation of marked bone loss around the implants Image of the large defect after the extraction of the implants Details of regenerated bone after the GBR therapy Appearance of the tissues once the regenerated bone had healed Appearance of the tissues once the regenerated bone had healed Checking the newly formed bone Biomimetic Iceberg Implant Placing the Biomimetic Iceberg implants View of the implants in place, with the polished collar at the transmucosal level View of the implants in place, with the polished collar at the transmucosal level Anodized healing abutments Anodized healing abutments Taking conventional impressions Definitive prosthesis in the mouth Definitive prosthesis in the mouth Details of the final zirconium prosthesis Details of the final prosthesis 1 year and 2 months after the restoration Details of the final prosthesis 1 year and 2 months after the restoration Periapical x-ray 1 year and 2 months after restoring the case