INTRODUCTION AND OBJECTIVES
Surgical treatment may often be the best therapeutic alternative in patients with class III malocclusion. However, the associated risks and surgical complications, together with the higher cost, must be taken into consideration. Non-surgical treatment should be considered if it can give comparable results, and may be the treatment of choice in some patients.
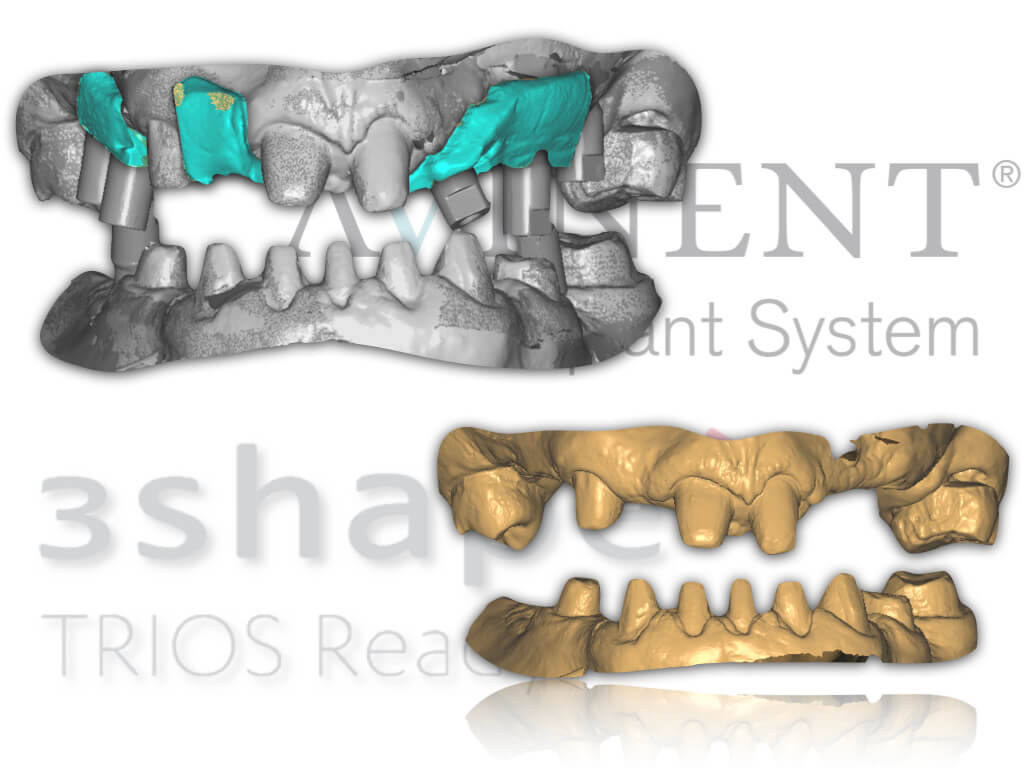
The aim of this study has been to perform a full oral rehabilitation including teeth and implants in a skeletal class III patient using digital work flow techniques. Our results show the effectiveness of complete-arch intraoral scanners to give the patient both a functional and aesthetic restoration without the need for orthognathic surgery.
METHODS
Patient who contacted the Master’s Degree in Oral and Occlusion Prostheses seeking an alternative to orthognathic surgery and orthodontics to rehabilitate his mouth. At baseline, he presented multiple dental absences and poor oral hygiene. His remaining teeth were in poor condition, and he presented agenesis of a mandibular incisor.

The first step was to determine the final vertical dimension (VD). Positioning the mandible in a centric relation (CR) showed that occlusion was practically edge to edge. In this case, the malocclusion was functional, since the patient thrust the jaw forward to avoid incisal interferences, giving rise to anterior crossbite. Based on these observations, we decided to rehabilitate in CR and increase the VD by 4mm with respect to the maximum intercuspal position.

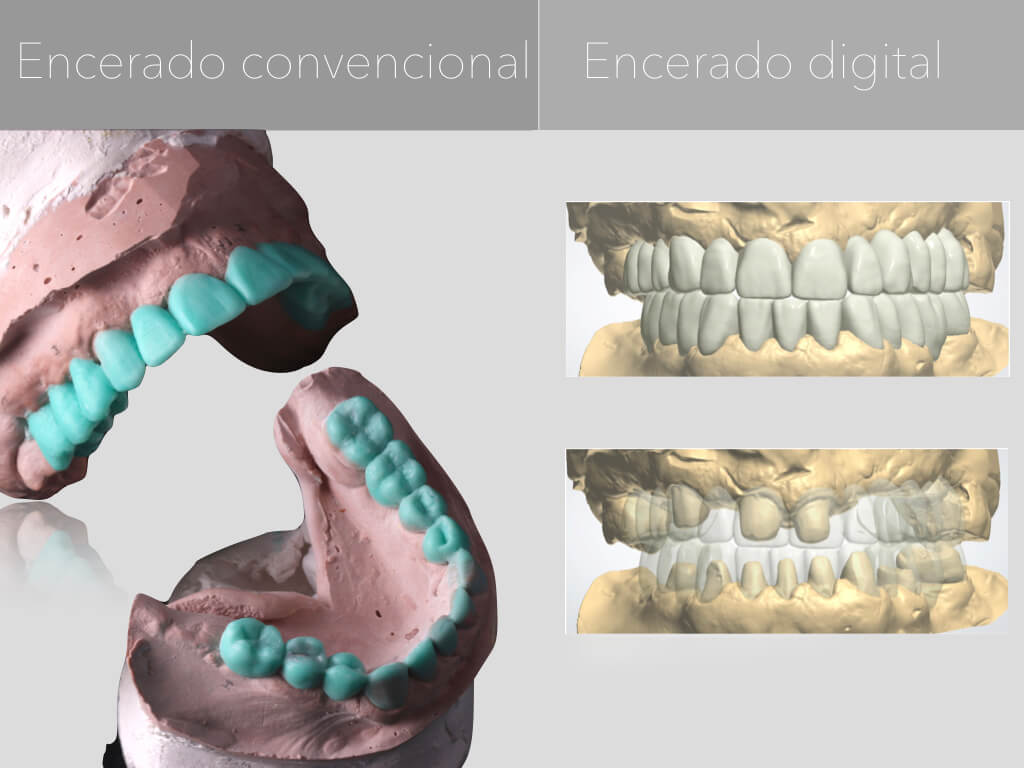
In this case, we decided to make a second virtual wax up using an earlier carving of the remaining teeth in order to obtain a more accurate view of the real outcome.

Our milling centre will make the metal rehabilitation structures, allowing us to customise the structures without modifying the structure of the material, facilitating ceramic build-up without distorting the final result. Milling structures on natural teeth or implants guarantees absolute precision and better passive adjustment of the structure than that obtained with cast or sintered structures.
EVOLUTION

It is important to find out the patient’s preference, and tell them when a less invasive treatment plan may be optimal. When performing a rehabilitation on a patient with malocclusion, it is essential to make a diagnostic wax up that will act as a guide through the preparatory, provisional and restorative phases. Using intraoral scanners, we were able to rehabilitate two complete arches with maximum precision, thus avoiding the errors typical of conventional impressions.
CONCLUSIONS
Once the patient has been fully informed of the therapeutic options, and chooses to avoid surgery or orthodontics, a restorative/prosthodontic approach can give an exceptional functional and aesthetic outcome. Although more studies are needed to show the accuracy of complete arch intraoral scanners, in this patient they proved to be an alternative to conventional impressions. This technique could improve efficiency, facilitate workflow, and minimise patient discomfort.