Introducción
A lo largo de los años, el uso del óxido de zirconio en las rehabilitaciones protésicas implantosoportadas ha pasado de coronas y pequeños puentes a rehabilitaciones completas. Por consiguiente, el reto de utilizar este material en grandes rehabilitaciones sobre implantes es conseguir una óptima pasividad para garantizar la durabilidad de la estructura, ya que estas tienen mucha rigidez y no toleran bien la torsión.
Actualmente, en detrimento de las prótesis completas monolíticas de circonia sobre interfases de titanio, se opta por el diseño de estructuras híbridas formadas por una estructura primaria y una secundaria personalizadas, con diferentes materiales, que permiten aportar mayor pasividad a la circonia y mantener la estética en la rehabilitación final. Soluciones innovadoras que permiten realizar grandes rehabilitaciones implantológicas de alta calidad, con un óptimo ajuste, durabilidad y alta exigencia estética con protocolos 100% digitales, a partir de tres conceptos clave: planificación protésicamente guiada, provisionalización inmediata simple y restauración final predecible.
En estos casos la gran dificultad radica, por un lado, en la obtención de una correcta pasividad de las estructuras a los implantes y, por otro lado, en repartir correctamente las cargas oclusales para que las fuerzas de la masticación sean soportadas por la estructura metálica de refuerzo. Esto no es sencillo ya que la distribución de los implantes en el paciente desdentado no siempre es ideal por la reabsorción ósea que acompaña a la desdentación. Conseguir una buena ubicación de la estructura primaria ayudará a garantizar la durabilidad de la supraestructura de óxido de circonio y el mantenimiento a largo plazo de la rehabilitación en boca.
Keywords: rehabilitaciones digitales, metal-circonia, nuevos conceptos y protocolos.
Presentación del caso
Paciente varón de 60 años, con desgastes funcionales, fumador con buena higiene bucal, con HTA, antecedentes de IAM leve unos meses atrás y riesgo ASA II. Acude a la consulta por fracaso de la rehabilitación dentosoportada anterior que llevaba desde hacía más de 15 años donde, por falta de soporte posterior y sobrecarga por el hábito bruxista, se fracturaron algunos muñones pilares que soportaban la prótesis.
Estado inicial del paciente Estado inicial del paciente Estado inicial del paciente
Tras un exhaustivo examen clínico, y ante la manifestación del paciente sobre la incapacidad de soportar una prótesis removible, se planteó una rehabilitación fija sobre implantes de arco completo.
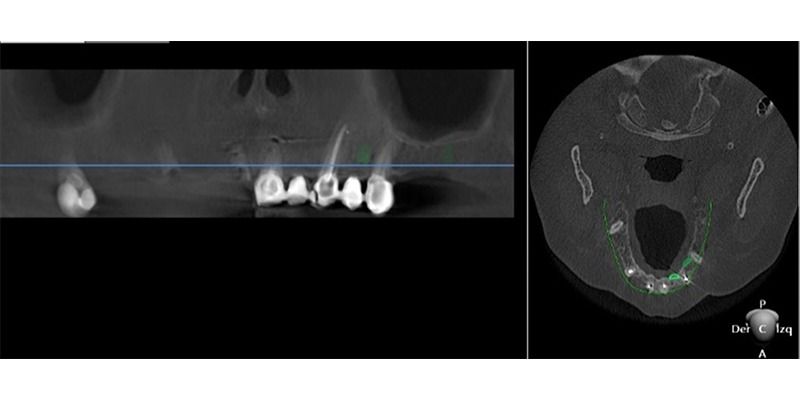
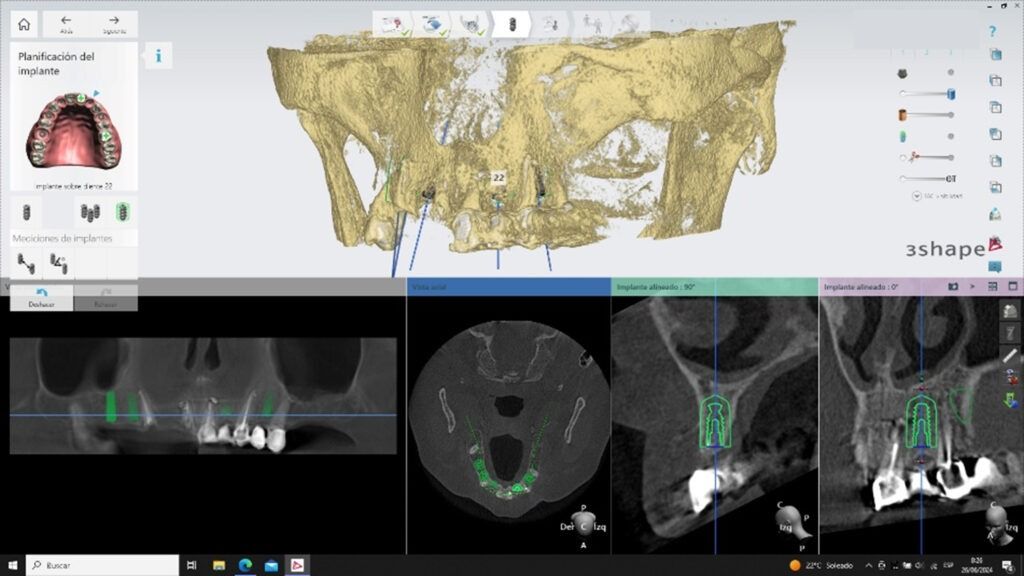
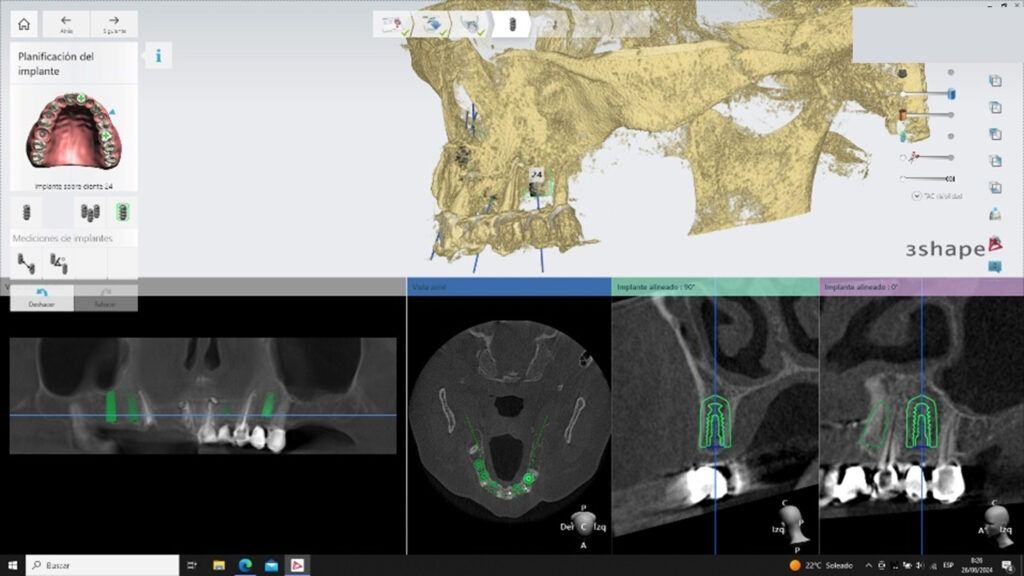
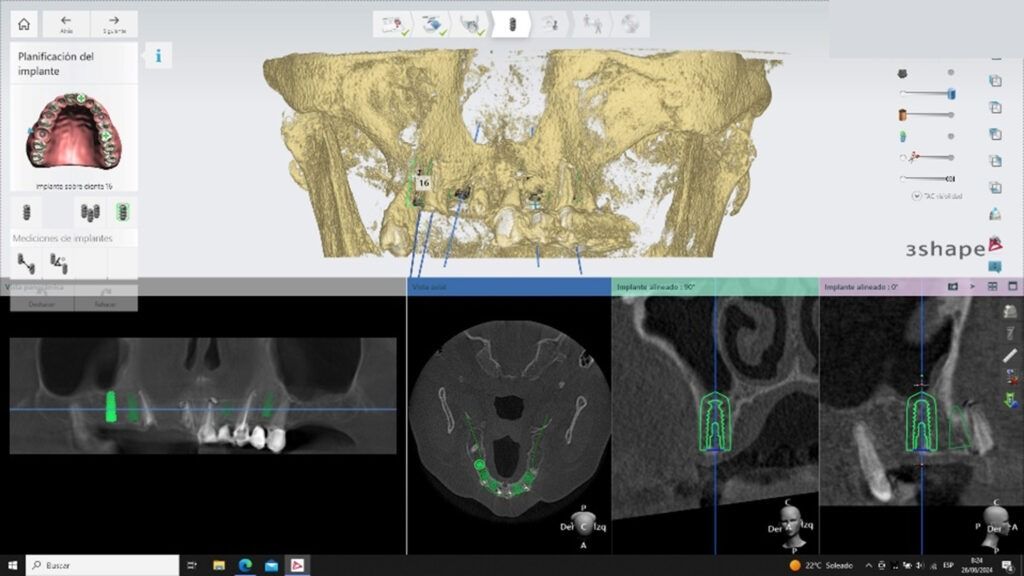
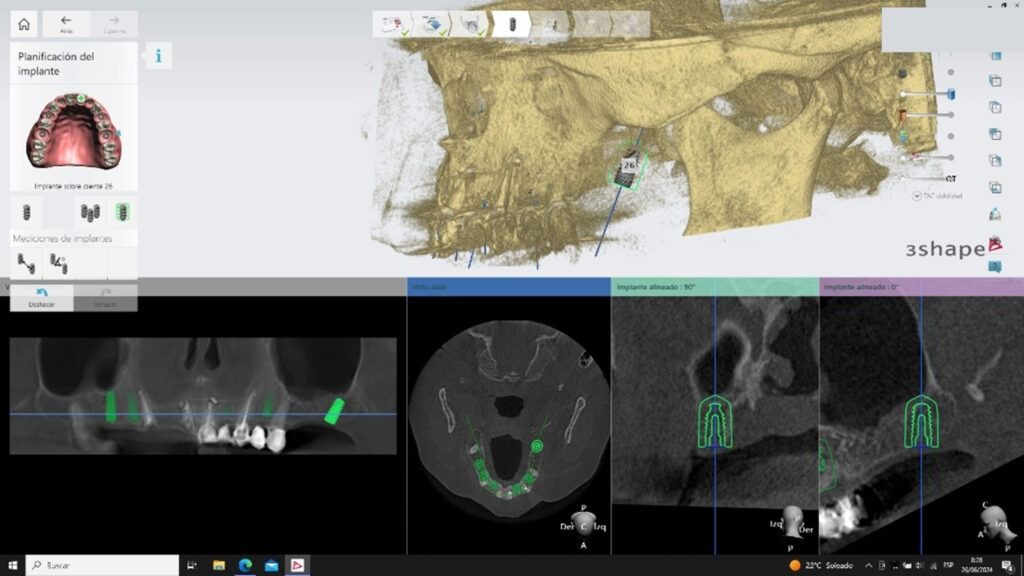
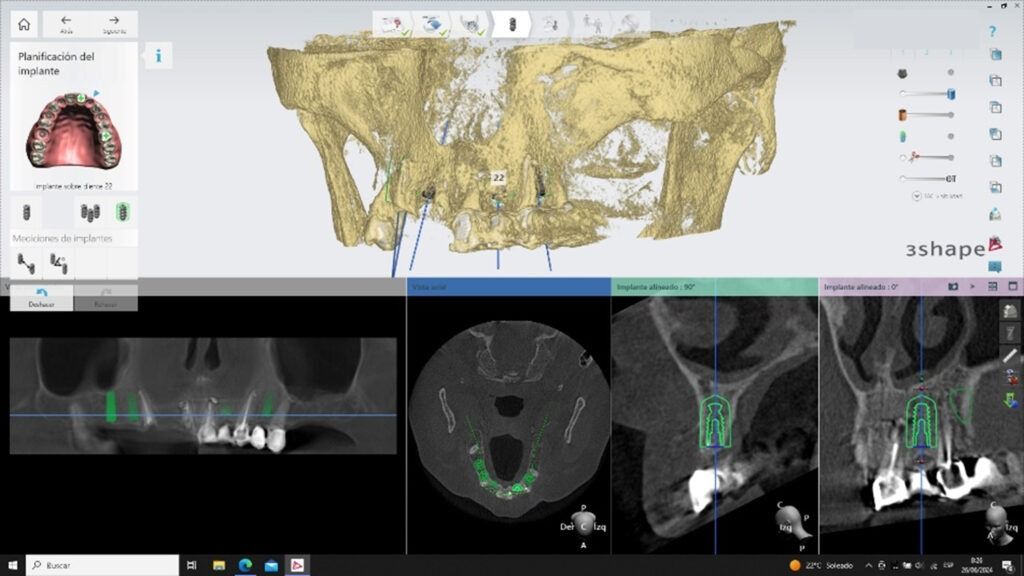
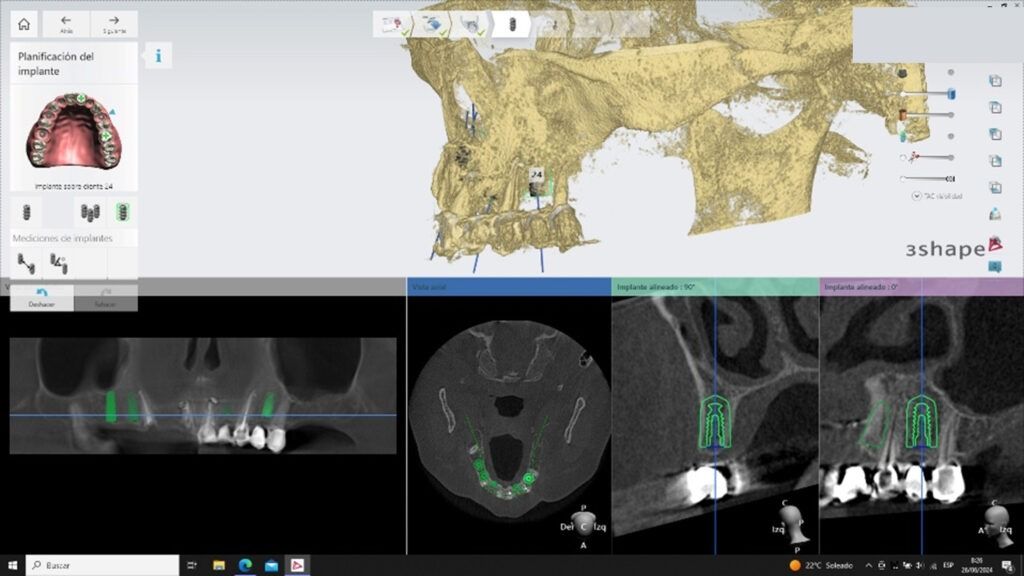
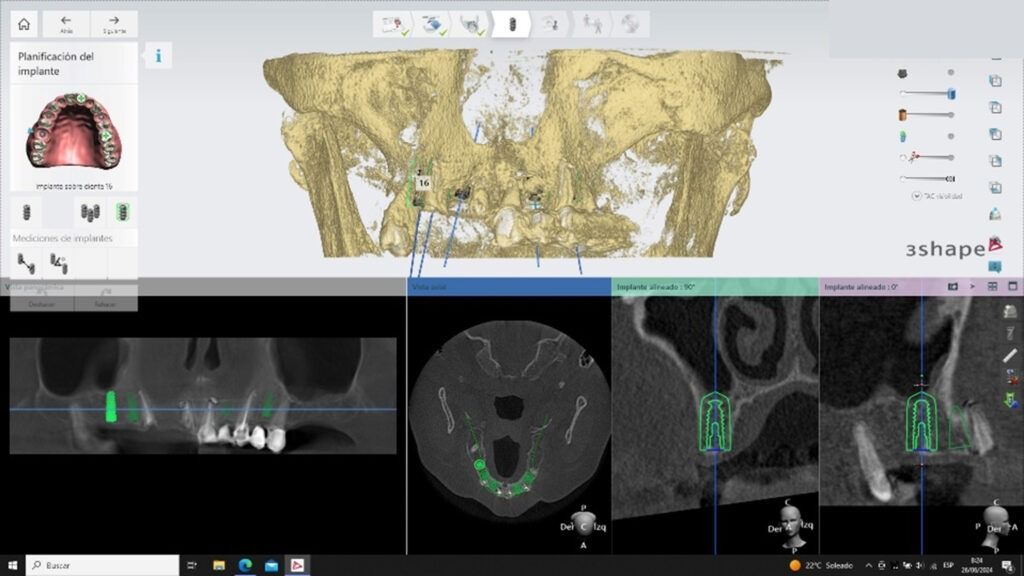
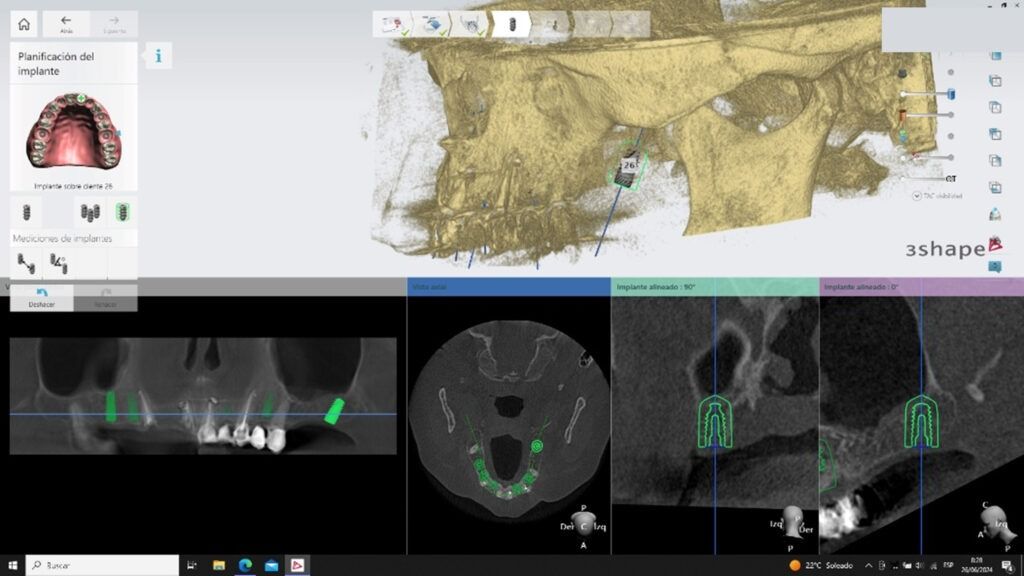
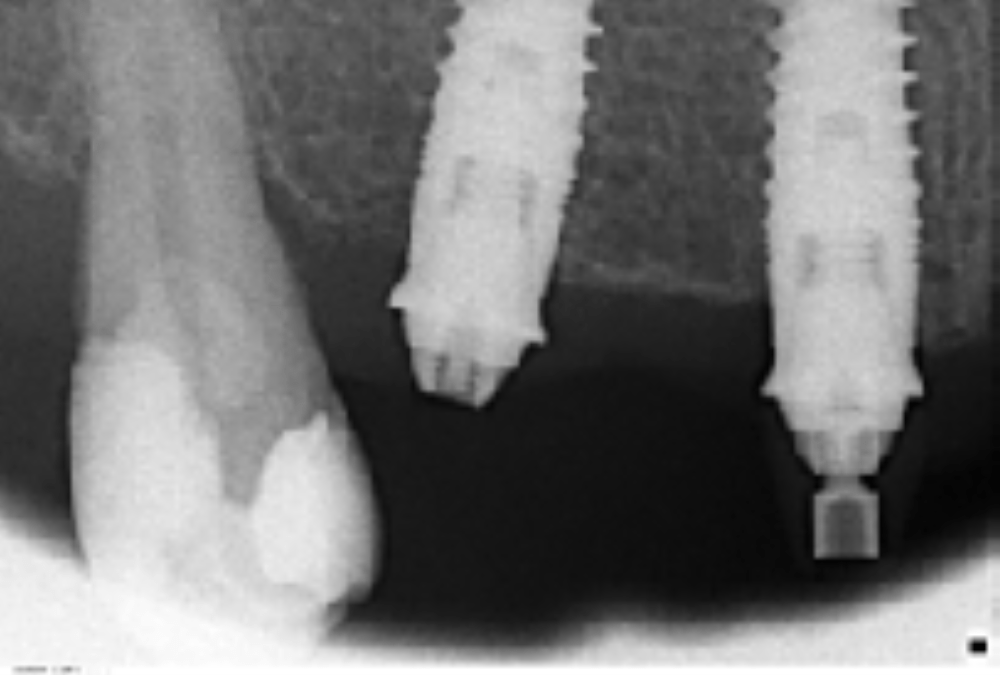
Aunque los implantes se colocarían manualmente y no mediante una férula de cirugía guiada, igualmente se planificó su distribución protésicamente guiada mediante el software Implant Studio de 3Shape. Se planificaron 6 implantes Biomimetic Iceberg CC.I en posición 12, 14 y 16 en el cuadrante superior izquierdo y 22, 24 y 26 en el derecho.
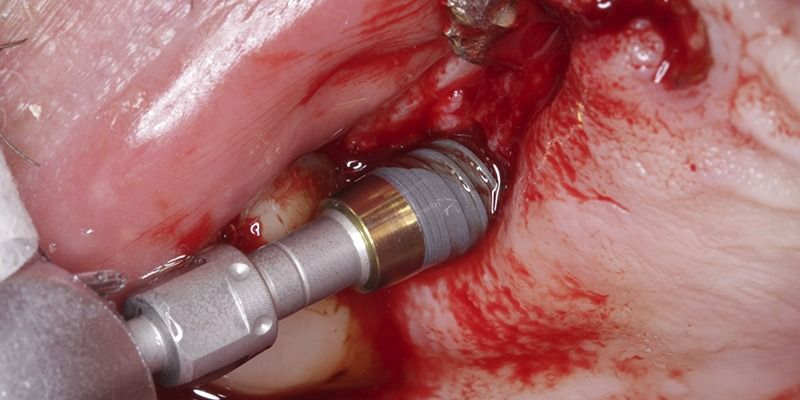
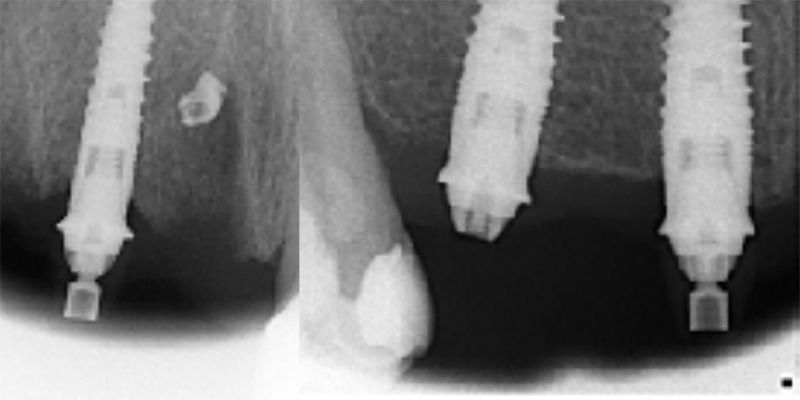
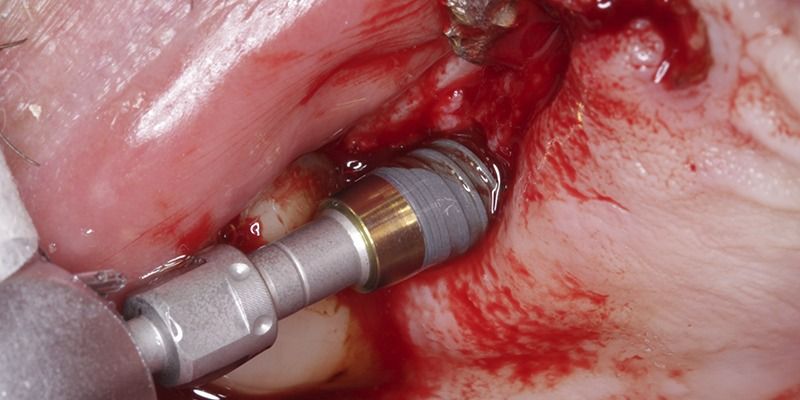
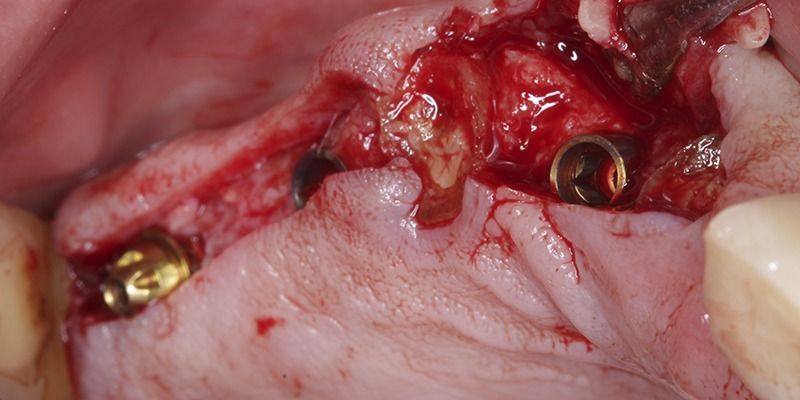
La fase quirúrgica se inició con la colocación de los implantes posteriores en ambos lados del maxilar superior, Biomimetic Iceberg CC.I de 4.0×10, 4.5×8.5 y 4.5×10 en posiciones 14, 16 y 26 respectivamente, pero al no obtener suficiente estabilidad primaria, se decidió posponer la colocación de los implantes de la zona anterior para una siguiente cita y, por supuesto, se descartó la carga inmediata planificada en un primer momento. El hecho de que el paciente presentara la desdentación posterior inicialmente facilitó la toma de decisiones, asumiendo el riesgo de que el resto de dientes anteriores pudieran claudicar durante el tiempo de espera a la cicatrización de estos primeros implantes.
Tras 16 semanas de la primera cirugía, fracasó de manera asintomática el implante de la posición 26.
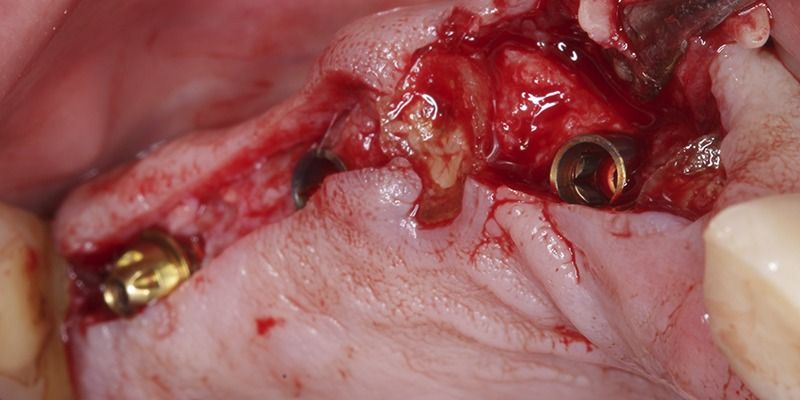
Aprovechando la segunda cirugía de colocación de los implantes de la zona anterior, en la que se colocaron dos Biomimetic Iceberg CC.I de 3.5×11.5 en las posiciones 22 y 24, se procedió a colocar un nuevo implante en posición 26 ligeramente a distal de la ubicación previa pero acorde con la planificación protésica inicial. Terminada la cirugía, se realizó una carga provisional inmediata sobre pilares transepiteliales de los implantes anteriores junto a los implantes colocados en la primera cirugía, pero sin incluir el implante en posición 26
Prótesis provisional en boca Prótesis provisional en boca Prótesis provisional en boca
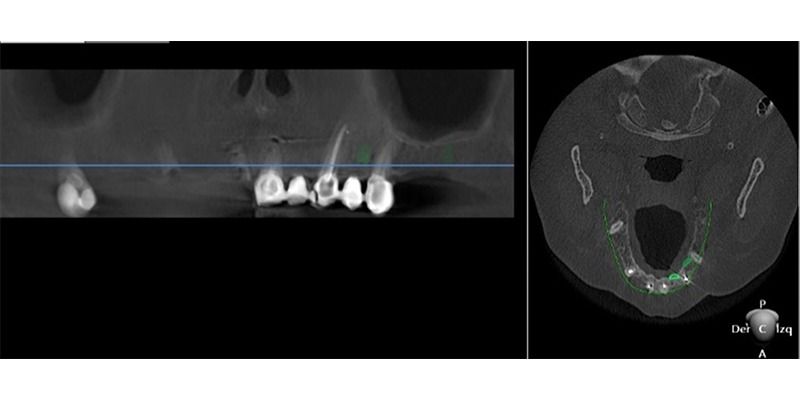
Pasado el tiempo oportuno tras la cirugía, se desmontó la prótesis provisional por primera vez y se observó que habían fracasado dos de los implantes del segundo cuadrante (22 y 24). El paciente, además de fumador, durante los meses de cicatrización de los implantes sufrió un segundo infarto; el primero lo había sufrido antes de la primera cirugía.
Se extrajeron los implantes fracasados, sustituyéndolos por dos más en la misma posición 22, en la 24 y se optó por colocar otro más en posición 21 dado que la cicatrización de esa zona había sido favorable y para evitar un tramo protésico demasiado largo y curvo en sector anterior. Se conectaron los implantes al provisional inicial y se volvió a esperar el tiempo de osteointegración necesario manteniendo siempre al paciente con una prótesis fija atornillada.
Imágenes del periodo de osteointegración de los implantes Imágenes del periodo de osteointegración de los implantes Imágenes del periodo de osteointegración de los implantes
Después de tantos problemas quirúrgicos, finalmente se consiguió la estabilidad necesaria para comenzar la fase protésica definitiva.
Se tomaron impresiones digitales con el escáner intraoral Trios (3Shape) para realizar una prueba a volumen total en plástico (PMMA) a partir del diseño del provisional que se hizo durante la primera fase y que tuvo que ser modificado en varias ocasiones. Una vez verificado el nuevo provisional de PMMA se pasó al diseño de la estructura primaria en titanio.
Detalles de la prótesis provisional implantosoportada fabricada en PMMA Detalles de la prótesis provisional implantosoportada fabricada en PMMA Detalles de la prótesis provisional implantosoportada fabricada en PMMA
Se diseñó una estructura primaria en titanio grado V, material biocompatible con un comportamiento biológico óptimo para el buen mantenimiento de los tejidos. La estructura de titanio se mecanizó, igual que las conexiones de los implantes, manteniendo el acabado totalmente pulido de la zona basal. Una vez validado el diseño de la estructura metálica, se procedió a diseñar la estructura de zirconio secundaria con un diseño anatómico y con perfiles más suaves.
Diseño de la barra primaria de titanio Diseño de la barra primaria de titanio
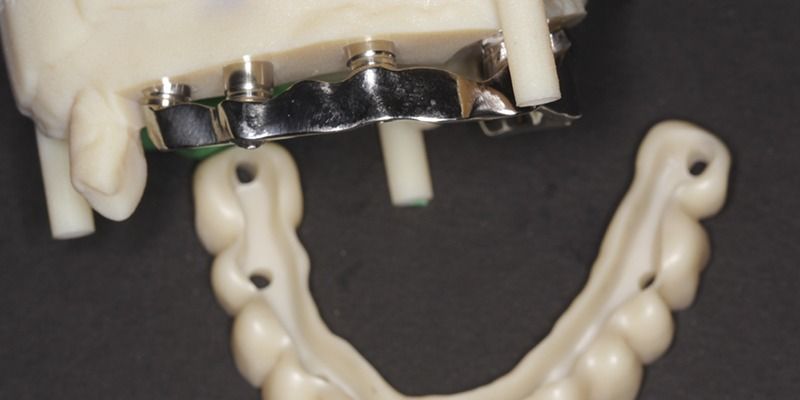
Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura Imágenes de la confección de la supraestructura
La estructura primaria actúa de interfase personalizada, mientras que la secundaria compensa con el diseño las zonas más débiles para que sea más homogéneo el resultado de la prótesis híbrida final y permita soportar los pequeños desajustes y micromovimientos entre el metal y el cemento.
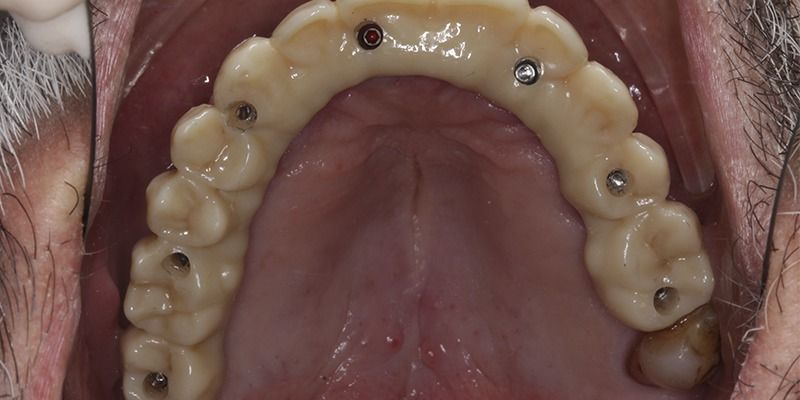
Diferentes vistas de la supraestructuras Diferentes vistas de la supraestructuras Diferentes vistas de la supraestructuras Diferentes vistas de la supraestructuras Diferentes vistas de la supraestructuras Diferentes vistas de la supraestructuras
Tras unos 6 meses después de la colocación de los implantes, se detectó una recesión gingival a nivel del implante 14. En un primer momento se pensó hacer un injerto, pero dado que el paciente tiene una línea de sonrisa baja y que no quería someterse a más cirugías, se decidió postergar la intervención y tenerlo en seguimiento.
Finalmente, a los 12 meses después de la colocación de los últimos implantes, se colocó la prótesis atornillada definitiva.
Resultado clínico del caso
La correcta planificación y la buena elección de los componentes que formaran parte del tratamiento implantológico son un punto muy importante para el buen resultado final del conjunto.
En este paciente, la geometría de los implantes Biomimetic Iceberg permiten alejar la conexión protésica de la unión hueso-implante y la zona transmucosa del cuello con perfil convergente favorece el sellado del tejido blando, manteniendo unos buenos niveles de tejidos periimplantarios, condición indispensable para el éxito del tratamiento a largo plazo.
La conexión cónica del implante Iceberg permite una mejor distribución de fuerzas, evitando la concentración de tensiones a nivel del tornillo y de la zona coronal del implante, tal como está ampliamente demostrado en la literatura. La colocación de pilares transepiteliales intermedios en una prótesis múltiple permite aprovechar el comportamiento biomecánico del implante cónico, facilitando la colocación y ajuste de grandes rehabilitaciones.
El nuevo diseño de supraestructuras híbridas en dos partes permite restaurar en circonio grandes trabajos con menor riesgo de fractura. Se trata de una prótesis cemento atornillada que tan buenos resultados aporta en las rehabilitaciones unitarias o parciales trasladado a arcadas completas, donde el riego de fractura aumenta por la dificultad de conseguir una pasividad perfecta. En este caso, debido a la dificultad de poder llevar a cabo una rehabilitación por sectores, nos veíamos obligados a realizar un arco completo de una pieza. Tanto por las ventajas técnicas como por la comodidad del paciente, se realizó todo el flujo digital, haciendo más sencillo el procedimiento de laboratorio reproduciendo el diseño digital con el material definitivo.

Conclusiones
Actualmente flujos digitales y nuevos materiales como el óxido de circonio (estético, funcional, resistente y biológicamente muy estable) permiten atornillar grandes rehabilitaciones sobre implantes gracias a nuevos diseños como las supraestructuras.
Estas soluciones innovadoras y funcionales permiten fabricar rehabilitaciones dentales de alta calidad, ajuste perfecto, gran durabilidad y alta exigencia estética.